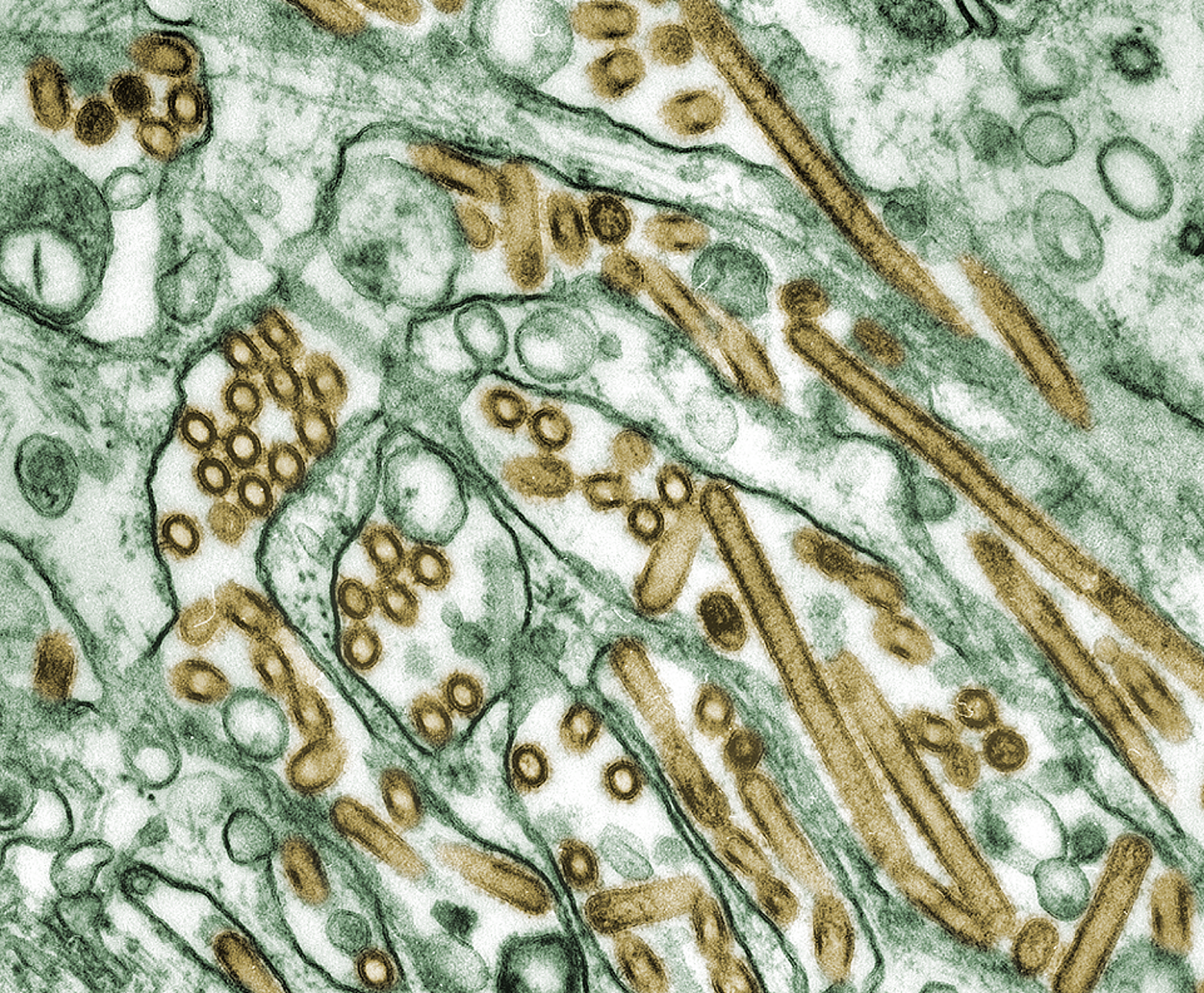
![]() When the media first caught wind that people had gotten sick with an Avian influenza virus, they began spreading fear about a global epidemic. The strain in question, H5N1, is devastating to birds. It's killed millions of poultry in Asia alone, and disease experts worried that close contact with infected animals might give the virus the opportunity to exchange genetic material with a human influenza virus, allowing the deadly avian flu to be spread person to person.
When the media first caught wind that people had gotten sick with an Avian influenza virus, they began spreading fear about a global epidemic. The strain in question, H5N1, is devastating to birds. It's killed millions of poultry in Asia alone, and disease experts worried that close contact with infected animals might give the virus the opportunity to exchange genetic material with a human influenza virus, allowing the deadly avian flu to be spread person to person.
 All and all, 248 humans have died from the H5N1 according to WHO data as of January 2009. H5N1, as a strain, infects more species than any previously known flu virus, is deadlier than previous strains, and continues to evolve becoming both more widespread and more deadly. But even still, fears of a pandemic have yet to be realized. Now, researchers might have found the reason: our noses are too cold for the Avian flu.
All and all, 248 humans have died from the H5N1 according to WHO data as of January 2009. H5N1, as a strain, infects more species than any previously known flu virus, is deadlier than previous strains, and continues to evolve becoming both more widespread and more deadly. But even still, fears of a pandemic have yet to be realized. Now, researchers might have found the reason: our noses are too cold for the Avian flu.
For a virus to infect both humans and birds, it has to overcome the differences between the two hosts. The first major barrier that prevents avian flu from infecting people is our cells themselves. Simply put, our cells are different than bird cells, and thus a pathogen needs different tools to gain access to them. The main fear, in terms of Avian flu, was that an avian virus would combine genetically with a human virus, thus giving it the right tools to get into our cells. Of the 16 subtypes of avian influenza, only some can mutate into forms that can infect humans, and those that do swap proteins on their surface with proteins from human influenza viruses. But even with the access granted, could the H5N1 virus become highly contagious and pathogenic in people? A new study, published in PLoS Pathogens, says not necessarily. It turns out that even combined human/avian flu viruses that can infect human cells don't reproduce well at 32 degrees Celsius, the temperature of our noses.
 The difference in temperature, internally, between a human and a bird isn't all that different - people maintain an internal temperature of about 37 degrees Celsius, whereas birds stay a little warmer, around 40 degrees Celsius. Researchers from the University of North Carolina wanted to know how these temperature differences might affect avian influenza viruses. They took an avian virus strain, H4N6, and human flu H3N2, and tried to infect human airway epithelial cells - the cells that line our noses and lungs. Both, they found, could infect and replicate quite quickly human airway epithelial cells at 37 degrees Celsius, though the avian ones were a little slower in general than the human ones. But when the temperature was dropped to that of our noses - a bit cooler 32 degrees Celsius - the avian virus replication slowed to a snail's pace, 3-5 log units below the human virus' speed. They tried a different avian strain - H5N3 - and found the same results. So they tried the deadly virus itself, H5N1 isolated from a dead person, and even it fared poorly. It seems that something about avian flu viruses simply can't function right in cooler temperatures.
The difference in temperature, internally, between a human and a bird isn't all that different - people maintain an internal temperature of about 37 degrees Celsius, whereas birds stay a little warmer, around 40 degrees Celsius. Researchers from the University of North Carolina wanted to know how these temperature differences might affect avian influenza viruses. They took an avian virus strain, H4N6, and human flu H3N2, and tried to infect human airway epithelial cells - the cells that line our noses and lungs. Both, they found, could infect and replicate quite quickly human airway epithelial cells at 37 degrees Celsius, though the avian ones were a little slower in general than the human ones. But when the temperature was dropped to that of our noses - a bit cooler 32 degrees Celsius - the avian virus replication slowed to a snail's pace, 3-5 log units below the human virus' speed. They tried a different avian strain - H5N3 - and found the same results. So they tried the deadly virus itself, H5N1 isolated from a dead person, and even it fared poorly. It seems that something about avian flu viruses simply can't function right in cooler temperatures.
But the researchers weren't done yet. Sure, the avian virus doesn't do well by itself at colder temperatures, but what about when it's crossed genetically with a human virus? That is, after all, the big fear. So the researchers combined the strains in a few different ways. They could speed up the transmission of avian viruses by giving them the same surface proteins that human viruses use. But they found that the mixtures were less effective than the human virus when they had certain avian proteins, and temperature was a major factor in their ability to replicate. Based on their data, the authors conclude that the data "substantiates differential host temperature as a critical barrier for infection by avian influenza viruses."
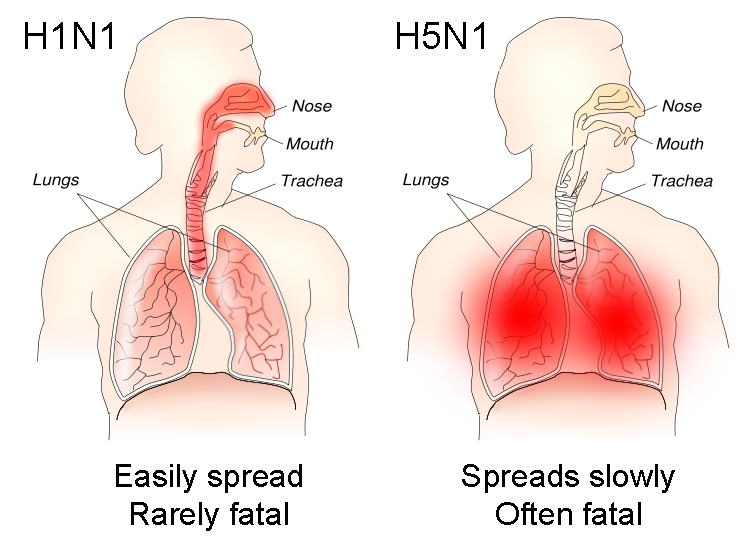 In other words, our noses are a bit too cold for avian viruses to replicate quickly enough to establish infection. This causes a major problem for the viruses, and is probably a big reason why they haven't evolved yet to transfer person to person. Our noses are a big infection site - we breathe in all kinds of foreign particles every day, and in our nasal passages, there is a constant struggle to prevent infections. If the avian viruses can't win that battle there, they have a lot more trouble infecting people. Those who have been infected by avian flu likely got particles deep into their lungs directly, where the warmer temperatures allow the virus full access.
In other words, our noses are a bit too cold for avian viruses to replicate quickly enough to establish infection. This causes a major problem for the viruses, and is probably a big reason why they haven't evolved yet to transfer person to person. Our noses are a big infection site - we breathe in all kinds of foreign particles every day, and in our nasal passages, there is a constant struggle to prevent infections. If the avian viruses can't win that battle there, they have a lot more trouble infecting people. Those who have been infected by avian flu likely got particles deep into their lungs directly, where the warmer temperatures allow the virus full access.
This doesn't mean that H5N1 won't become an epidemic flu. It still could mutate and get enough genetic information to overcome this obstacle. But it does mean that it's a little harder than we thought for the deadly virus to do so - which, as far as I'm concerned, is good news. It also helps us better understand which strains are closest to bridging that gap, and thus which ones are the most dangerous and likely to lead to an outbreak. By using the model in this study, scientists could see which animal viruses are able to spread well at the lower temperature threshold, and those that do might be on the verge of jumping into humans. Instead of worrying about every possible danger, we can target our vaccine and quarantine efforts to those that pose the highest risk, saving us valuable time and money in the fight against disease.
Scull, M., Gillim-Ross, L., Santos, C., Roberts, K., Bordonali, E., Subbarao, K., Barclay, W., & Pickles, R. (2009). Avian Influenza Virus Glycoproteins Restrict Virus Replication and Spread through Human Airway Epithelium at Temperatures of the Proximal Airways PLoS Pathogens, 5 (5) DOI: 10.1371/journal.ppat.1000424
- Log in to post comments
