If there's a topic that I don't write about much, it's obstetrics. The reason is that it's not a major area of my interest, and it's not an area where I have as much expertise as I do in, say, cancer or even vaccines. My expertise in cancer comes from my career, of course, and my expertise in vaccines is self-taught through my 9+ years of blogging about it. Ditto my expertise in "complementary and alternative medicine" (CAM), also known as "integrative medicine," about which I know quite a lot now. That's probably why I didn't pay much attention to a study that came out in late January from the The Midwives Alliance of North America Statistics Project, 2004 to 2009 (MANA). However, this study came to my attention due to a little blog kerfuffle going on between Dr. Amy Tuteur, who goes by the blog moniker The Skeptical OB (or Dr. Amy) and Jamie Bernstein over at Grounded Parents. Fortunately, the paper is available online; so we can all follow along, which allows me to do what I think best, discuss the paper first and then the blog kerfuffle, which, to be honest, I'm having a hard time figuring out why it's become so vitriolic. It's actually rather disturbing to see, given that the differences in position seem rather small. Going through it all, as painful as it is, might be educational. Besides, I've already pissed off one big name skeptic a couple of weeks ago. If I end up pissing off another one, it's no big deal at this point, right?
Right.
Besides, one of the parties involved in this little dustup (which is, sadly, kicking up a fair amount of dust), Jamie Bernstein, who's a friend of mine, asked me to look into the issue. At first I didn't want to, but I changed my mind.
Before I go on, let me just say also that I tend to agree that most of the time home births are probably bad idea. There's a lot of evidence out there that the risk to both mother and baby from home birth is significantly higher than it is in hospital. While it might be possible in highly selected cases to justify doing a home birth for low risk singleton pregnancies, it strikes me as way too risky to consider a home birth for higher risk, complicated pregnancies. Actually, this study suggests the same thing. Finally, I have noted that there is very much a cultish aspect that has grown up around home births, where the risks are downplayed and the "experience" is all. These are the areas where Dr. Amy, Jamie, and I generally appear (mostly) to agree, all the more reason why I'm puzzled by this whole thing.
The MANA study
First, let's take a look at the paper. No, wait. First, let's take a look at what MANA said about the paper in its press releases and fact sheets:
Safe Outcomes with Positive Benefits
- High rate of completed home birth (89.1%)
- High rate of vaginal birth (93.6%)
- High rate of completed vaginal birth after cesarean (VBAC; 87.0%)
- Low intrapartum and neonatal fetal death rate overall:
- o 2.06 per 1000 intended home births (includes all births)
- o 1.61 per 1000 intended home births excluding breech, vbac, twins, gestational diabetes, and preeclampsia.
- Low rate of low APGAR scores
- Extremely high rate of breastfeeding (97.7%) at 6 weeks
Few Emergency Transfers to Hospital Care
- Primary reason for transport was “failure to progress.” Transfer for urgent reasons, such as “fetal distress” was rare.
Low Rates of Intervention
- Cesarean section rate of 5.2%
- Less than 5% used pitocin or epidural anesthesia
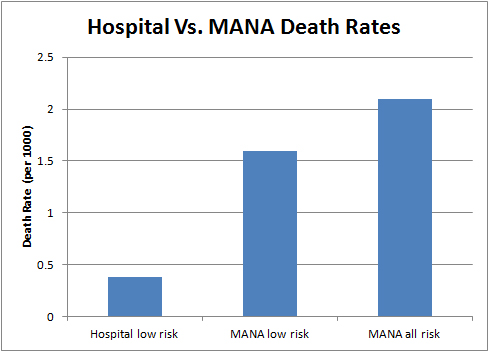
Sounds fantastic, doesn't it? There's just one problem, which has been pointed out by Dr. Amy, Jamie Bernstein, and Steve Novella. That problem is that, if you compare the death rates in the MANA study to publicly available death rates from other sources, the death rates in the MANA cohort are higher—and not just by a little. The issue behind the fracas is how much higher and in emphasis.
Actually, the better way to describe the problem with this study is that there is no control group. This is a single arm, prospective study. It's good that it's prospective, rather than retrospective, because it means that the data were all collected as patients were enrolled. However, it's also important to recognize that this is not a typical group of pregnant women giving birth. As the authors themselves mention in the introduction that 1.18% of births in the US occur outside of the hospital, and, of those, approximately 66% are homebirths, for a total of 31,500 home births a year. This study examines 16,924 pregnancies, for a total of 16,984 neonates including 60 sets of twins, over birth years ranging from 2004 to 2009, which breaks down to around 3,385 births a year, a bit more than 10% of the home births estimated to have occurred in the US during this time period. That's a significant sample, but it's nonetheless a small fraction of an even smaller fraction of all the births that occurred in the US during that time frame.
That this is an unrepresentative sample is obvious just perusing the numbers, which are overwhelmingly white (92.3%) and college-educated (58.4% having completed a college degree, compared to 33.5% recently estimated for the general population). Basically, the numbers were what the press release/fact sheet listed above. Other important numbers were summarized here:
The overall death rate from labor through six weeks was 2.06 per 1000 when higher risk women (i.e., those with breech babies or twins, those attempting VBAC, or those with preeclampsia or gestational diabetes) are included in the sample, and 1.61 per 1000 when only low risk women are included. This rate is consistent with some published reports of both hospital and home birth outcomes, but is slightly higher than others. Because only 0.45 per 1000 separates these samples, further work is needed. These findings should, however, help to inform the process of shared decision-making as women talk with their providers about their own specific risk profiles, value systems and priorities for birth.
This leads the authors to conclude in their paper:
For this large cohort of women who planned midwife-led home births in the United States, outcomes are congruent with the best available data from population-based, observational studies that evaluated outcomes by intended place of birth and perinatal risk factors. Low-risk women in this cohort experienced high rates of physiologic birth and low rates of intervention without an increase in adverse outcomes.
Except, as Steve Novella pointed out, based on Dr. Amy's calculations, the equivalent number for the overall death rate from labor through six weeks for planned hospital births is 0.38 per 1000. Now, I fiddled around with the CDC Wonder Database a while trying to see if I could replicate Dr. Amy's number. I couldn't. There are lots of settings in the Wonder Database, and I tried to match the cohort in the MANA study as well as I could. No matter how I tried to do it, my numbers came out around 0.5 per 1000 or I got a lot of "suppressed" data, which apparently means that there were too few to be considered valid. As far as I'm concerned, that's close enough, as I didn't have time to fiddle with the settings all night last night and unless Dr. Amy reveals the exact settings she used to get her number, there's no way for me to easily replicate it easily. So, because it's simpler, I'll just assume she knew what she was doing and go with it. I also note that it's not possible to get death rates for birth and the six weeks after birth using the MANA database, because the choices do not include the first six weeks. The ranges are (1) under one hour; (2) 1-23 hours; (3) 1-6 days; (4) 7-27 days; and (5) 28 to 364 days.
Be that as it may, for low risk pregnancies, the MANA death rate of 1.61 per 1000 is 4.2 times higher than the estimate provided by Dr. Amy from the CDC database of 0.38 per 1000. If we use my quick and dirty estimate of 0.5 per 1000, then that's 3.2 times higher. Both of these numbers are within the range of what previous data have shown. For example, a meta-analysis from 2010 concluded that planned home births were associated with a tripling of the neonatal mortality rate. That's, as I would put it, plenty bad, man.
Of course, there are problems with this comparison. We're comparing apples and oranges in that there was no control group for the MANA study, and it's always problematic to compare what is in essence such a highly self-selected group with population-based statistics. We have no idea if the MANA group was representative of women who choose home births, because it's a group of women who not only chose home birth (less than 1% of pregnancies) but were also willing to sign the informed consent form to be in the study. Moreover, the error bars were large. Even when two groups are not easily directly comparable, as is the case here, a more than four-fold relative risk of death is definitely something to be concerned about, and it's concerning that MANA does its best to de-emphasize it.
In its Consumer Considerations, MANA tries to downplay the risk, and, to be fair, it does have (somewhat) of a point in that it points out that what we are talking about are relative risks. As Steve Novella points out, when you look at a comparison of absolute risk, the difference between home birth and hospital birth is 0.123% (0.161% -0.038%), or 1.2 per 1,000, estimating that in the study population this amounts to 20 extra perinatal deaths. I liken this to the issue of mammography and an example I used before:
Essentially, mammography reduces the odds of a 60-year-old woman dying of breast cancer in the next decade by 30%. Sounds impressive, until you look at her absolute risk: by getting her annual mammogram, her chances of dying from breast cancer are whittled from 0.9% to 0.6%. Overall, for every 1,000 women in their 60s screened for breast cancer in the next 10 years, mammograms will save the lives of 3 people but 6 others will still die. (The numbers edge up or down in lockstep with a woman’s age.)
The point is not to try to directly compare the numbers but to choose an example to illustrate a similar point, namely that when you look at absolute risks instead of relative risks, the perspective changes. I think it's important in these studies always to include both numbers, the relative risk and absolute risk. None of this excuses MANA from using the graphs they did to try to downplay the even more elevated risk of infant death in infants presenting in breech position or women undergoing a vaginal birth after Caesarean section (VBAC), which were 5 out of 222 and 5 out of 1052, respectively. What is being weighed is whether the value of the experience of home birth is worth the roughly three- or four-fold increased risk of neonatal death, which translates to approximately an extra 1 in 1000 chance of the baby dying. I'm not going to touch that one with the proverbial ten foot cattle prod except to say I'd conclude: No.
Unfortunately, there are not a lot of high quality comparative data to use. A recent Cochrane review concluded that there is "no strong evidence from randomized trials to favor either planned hospital birth or planned home birth for low-risk pregnant women." Of course, this is not surprising. Such a trial would be fraught with ethical difficulties, not the least of which because of data like the MANA data suggesting that home birth is almost certainly riskier than hospital birth. Moreover, from a strictly practical standpoint, I don't see too many women being willing to be randomized either to hospital or home birth. Observational evidence is what we are going to have to use, because it's highly unlikely that we'll ever have decent evidence from a randomized trial. For some questions in medicine, it has to suffice.
The Kerfuffle
The entire blog kerfuffle that's been intermittently flaring up boils down to a single graph and a single passage in Dr. Amy's post about this paper. Given how much I harped on certain skeptics to provvide full disclosure, I will state right here, right now, that Jamie asked me to look at these posts. So I did. Now here's the single graph:
And here's the passage:
As the chart above demonstrates, the MANA death rate for the same years was 5.5X HIGHER. In other words, the MANA death rate was 450% higher than the hospital death rate.
On what planet is a death rate 450% higher than expected a safe outcome? Not on this planet.
MANA and homebirth midwives have been lobbying extensively for a scope of practice that includes breech, twins, VBAC, etc. Now they want to exclude those same births from their statistics. Even then, the MANA death rate is 4.2X higher than hospital birth. So even when homebirth midwives stick to low risk patients, homebirth has a death rate 320% higher than comparable risk hospital birth.
One thing that's clear is that the figures of 2.06 per 1000 and 1.61 per 1000 were not in the MANA paper, at least not in that form. They were in that form in the Consumer Considerations page that I cited above. This clearly confused Jamie at the time because she couldn't find the equivalent numbers in the paper. I must admit that at first it rather confused me a bit, too, as to how those numbers were calculated based on the figures reported in the paper. I had to figure it out by wading through the data and determining which numbers had been added together to come up with these figures. Be that as it may, Jamie was critical of Dr. Amy for the above passage, for these reasons:
Let’s leave this study for a bit and go back to the numbers Dr. Tuteur cites in her post. According to Dr. Tuteur, 1.6 per 1000 low-risk planned homebirths from the recent study resulted in neonatal death within 6 weeks of birth. Using CDC data, she also determined that the risk of neonatal death for low-risk white women in the US during the same years was 0.4 per 1000 births. She then points out that OMGZ YOU GUYS THAT’S A 5.5X INCREASE IN BABY DEATHS!
First of all, can I first point out that it’s a 4x increase, not 5.5x (1.6/0.4 = 4). Even comparing the homebirth cohort that includes high-risk births (2.1 in 1000) to the low-risk only CDC cohort (which is not a fair comparison for obvious reasons) would only result in a 5.25x increase in mortality. I seriously have no idea how Dr. Tuteur came up with 5.5x or 450% increase in mortality from the numbers that she cited.
I can find no flaw in this reasoning, and, had I noticed this first, I would have been far more snarky about it, because, well, that's how Orac rolls. Dr. Amy should appreciate that, because she herself is often as sarcastic or more so than Orac is, only nowhere near as funny about it. Dr. Amy clearly did not do the right comparison, which would have been to compare low risk with low risk—by her own numbers. If she was so convinced that the figure of 2.06 per 1000 was the correct figure, then why did she include the figure of 1.61 on the graph and label it "low risk"? Moreover, her rationale makes no sense. After all, the statistics are right there, in the paper. True, they're not in a nice table format, like most of the other statistics presented in the MANA paper. But they are there, so much so that Dr. Amy was able to come up with 2.06 and 1.61 out of 1000 numbers by adding together the appropriate figures. In any case, Dr. Amy attacked Jamie's analysis as a "hatchet job." Some of what she says makes sense, but I'm going to cite one thing that is a steaming pile of fetid dingo's kidneys:
Clearly she never bothered to look at the CDC Wonder database, which contains an complete description of contents. I specifically noted that I looked at white women, 37+ weeks, 2500 gm babies.
No, Dr. Amy did not mention any such thing, at least not in her original post discussing the MANA paper. In any case, unlike Jamie, I did look at the CDC Wonder Database. I wasted quite a bit of my time fiddling around with it, trying to replicate Dr. Amy's number. I couldn't do it, because I was largely guessing based on what Dr. Amy said in her original post, "According to the CDC Wonder database, the neonatal death rate for low risk white women at term from the years 2004-2009 is 0.38/1000." Nope, there's nothing there about 37+ weeks or 2500 g babies. Armed with this new knowledge from Dr. Amy, I went back into the CDC Wonder Database, and plugged her figures in. That resulted in a mortality rate of 0.57 per 1000. At this point I was tempted to appeal to Dr. Amy for all of her other settings she used to search the CDC Wonder Database because I'm not getting the same number she is, and it's not because I can't figure out how to use the database. I use databases like this one all the time. But then I came across her a later analysis, I realized that the reason for the anomaly is probably because I didn't exclude the ICD-10 code for major congenital malformations from the causes of death. So I did it again and came up with an estimate of 0.34 per 1000. That's better, but still not identical to what Dr. Amy came up with. At least it's now close enough that I'm not wondering as much as I was before what the heck was going on. Still, it would be nice to know the full settings used.
I don't really want to go into the next phase of this little kerfuffle, which involves a statistics professor guest posting about the MANA study and a critique by Jamie, because this post has already grown too long, even by Oracian standards. Maybe if there's interest on your part (and still on my part) I might take it on another time. Whatever mistakes Jamie might have made (and it's clear that she didn't find the figures used to come up with the aggregate estimated mortality rates of 2.06 and 1.61 per 1000), she didn't deserve what came about a week ago, when this whole kerfuffle culminated in a rather amazing post by Dr. Amy that asked Can women be skeptics? In it, she says:
I’m beginning to wonder if there is a germ of truth to the claim that there are not more women in skepticism, because women are so anxious to avoid confrontation.
And:
You cannot be a skeptic and censor debate. Yes, you can remove racism and other evidence of hatred or discrimination. Yes, you can remove comments that are not on point. But you can’t censor comments that you don’t like and still call yourself a skeptic.
Say what?
Remember that there was a time when Dr. Amy was on Science-Based Medicine. It didn't work out. You want to know the reason it didn't work out? A certain guy that you all know and (hopefully) love described what happened in a comment:
Of course, Amy is free to present her side of the story as much as she likes on her blog. For now, we are going to take the high road and not get into a “he-said-she-said” sort of exchange. However, since Amy has cited our moderation policy as a reason for her departure, I no longer see a reason not to confirm that one unresolvable issue was that Amy strongly favored a more heavily moderated commenting system, and Steve and I were very reluctant to change our commenting policy. But the disagreement over the commenting system was certainly not only the bone of contention that we could not resolve.
Many of our regular readers will know who wrote that, but in the interests of full disclosure I'll just say: Here's another clue for you all. The walrus was Paul. No, wait, that won't do. Besides many of my readers being too young to get that reference, it's just another bad Orac joke. So instead let's just say that everybody's box of blinky lights wasn't too far at all from that particular comment, lo, those four years ago. (Has it really been that long?)
In any case, Dr. Amy clearly left SBM in part because she didn't like its free-wheeling, hands-off moderation policy (which is only marginally tighter than almost non-existent moderation policy here). I remember it well and could elaborate further, but I won't, at least not without a very compelling reason. What was written then says enough for my purposes.
The bottom line according to Orac
Here's what I don't understand. A four-fold increase in mortality in planned home births attended by midwives, if accurate, is plenty bad enough. It's more than enough to have grave concerns about the safety of even low risk births in the US. I say "if accurate," because comparisons between two such different sources are always fraught with issues because we don't know how comparable the groups are. However, a four-fold or five-fold increase in risk is enough that it starts to raise red flags, even accounting for the problems in comparing two different data sets.
So why does Dr. Amy have to make a questionable comparison—and, contrary to her defense of it, it is dubious—to get the risk up only to a 5.5-fold increase? I don't know. Compare low risk to low risk or all births to all births, but don't compare low risk to all births. I could understand the temptation if it meant the difference between a four-fold and a twenty-fold increase, but making a big deal out of the difference between a 4.2-fold and a 5.5-fold increase in the risk of neonatal death strikes me as pointless, given the size of the confidence intervals involved. We're all agreeing that there appears to be a significantly elevated risk of neonatal death due to home births. We're all agreeing that the mortality rate for breech presentation and other high risk pregnancies appears to be elevated in the MANA data to a very worrisome degree, making MANA's lobbying for a greater scope of practice for midwives to include these sorts of high risk pregnancies a policy to be opposed until there is evidence showing that their outcomes are equivalent. If this argument isn't about how many angels can dance on the head of a pin, it's not too far off from that.
So why all the vitriol from Dr. Amy? (Yes, it's mostly coming from her.) It doesn't make sense to me, particularly her bringing gender, rather than data, into the issue with her unnecessary insinuation that some women can't be skeptics because they're too touchy-feely and concerned about not offending—after her demands for an apology. Being civil and being a skeptic are not mutually exclusive. In other words, you don't have to be a jerk to be a skeptic, although clearly some skeptics are jerks at times, this box of blinky lights included, and some are jerks much of the time. Moreover, one can't help but note that Steve Novella came to the same conclusion that Jamie did long before I looked into this matter; yet I haven't seen him criticized the way Jamie was.
I suppose Dr. Amy won't be happy with me for writing this. I rather expect that I'll be accused of standing up for a friend (as if this were a bad thing), that somehow I don't "understand" the data; that I'm too stupid to figure out how to replicate Dr. Amy's search of the CDC Wonder Database, and the like. So be it. It's not as though I haven't endured far worse criticism over the years, sometimes even from people on "my" side. Who knows? She might even convince me that she's right and I'm wrong. Data can do that.
- Log in to post comments

For someone who's big into disclosing Conflicts of Interest, you wait an awful long time, about 3000 words in, to admit that you have a big beef in this fight yourself beyond "one side asked me to look into this". Puts the whole well argued part above in a cloud that wasn't needed.
Not arguing the rest, I'd say any evidence of a 100 % increase would be plenty to persecute every "planned home birth" for child endangerment.
Except that I don't have a big beef in this fight. I know Jamie Bernstein. She asked me to look into it because she wondered if she was wrong. We're not close friends, but we have met before a few times and we do know each other. We correspond sometimes about various skeptical issues. When I'm in Chicago, I like to hang out with the Chicago Skeptics if I have a chance, and she's usually there when that happens. That's about it.
As for that stuff with SBM from four years ago, it's ancient history. Everyone involved has moved on, and I hadn't really even given a thought to it until I became aware of this kerfuffle. Indeed, I never would have even mentioned it if Dr. Amy hadn't written that ridiculous post about some women "suppressing" criticism because they don't want anyone offended, and the reason it's so far in is because, well, it's not really that important to the overall issues I was discussing. Rather, it was simply a point worth knowing if someone has accused someone else of suppressing debate through overly vigorous moderation of comments.
If it makes you happy, I'll add a mention that Jamie's a friend of mine early on. You're actually probably right. I probably should have mentioned it right off the bat, but I don't think I needed to mention the SBM thing right off the bat because, well, it's such a minor part of the post as far as I'm concerned.
Orac...The reason people in the SOB camp are getting pissy is because Jamie was sloppy and also misrepresented 3 different people's positions. Dr Amy, Dr Orsosz and Esther Inglis-Arkell, the author of the i09 paper. She also hid behind moderation as GP quit allowing many comments pointing out her errors through. None of the ones I saw were abusive or violated the TOS. And obviously GP loves this click bait as they've posted shitty little responses to continue fueling the fire as well.
Not gonna lie, not impressed with them. I also agree that Dr Amy hurt her credibility by doing the math the way she did, but supporters of homebirth wouldn't find her credible if she said water was wet, either. Either way, the conclusion is the same. Does that excuse it, nope. But there's serious issues with homebirth in the US that deserve addressing. One unnecessarily dead baby is too many.
Further I find it very fascinating she asked her to mighty mouse for you and you agreed. Hmm. I have a huge nerdcrush on you and may have done the same, but I wouldn't expect you to actually do it.
And by io9 paper I mean article or blog post lol.
For whatever it's worth, my essay was directed NOT at Bernstein, but at the absurd assertions of certain home birth advocates, such as, "The MANA paper proves home birth is safe," and "The MANA paper proves home birth after Caesarian is safe." (Yes, I've seen the first repeated over and over again, including in the mainstream press, and the second repeated several times.)
Going to do something actually useful now, y'all have fun.
Oh my comment is so full of errors...'I find it very fascinating she would ask you to' is what it should say.
FYI the link to the PDF in the bolded words (just below the text you cite from Dr Tuteur's post, itself below the graph) is borked.
Dr. Amy is well known not only for vicious personal attacks on everyone who disagrees with her, but for making putative statements of fact that are unsupported or outright false. She probably objected to a moderation policy that did not allow her to delete comments that pointed out her numerous errors.
I think it's worth asking why studies from European countries in which home birth for low-risk women is much more common do not show a similar increase in neonatal or early mortality. Is this a question of correlation in America not being causation, or are the Dutch, etc. doing things better than we are, in which case we should adopt their practices?
You're certainly right that home birth seems unwise for high-risk women. However, women with breech or twin babies or prior C-sections who choose that option relatively often do so because they are afraid of being subjected in hospitals to coerced and outright forced Cesarean sections. What someone like Mu who would throw all home-birthing women in prison misses is that women, as well as babies, have legitimate interests. While hospitals might be slightly safer for babies in the short term (ignoring the later allergies, etc. associated with unnecessary C-sections), they are a lot more dangerous for women. At some hospitals more than a third of all women giving birth are subjected to major abdominal surgery, with significant physical and financial consequences, and a third of those will have some level of complications. For the entirely child-centered, growing up poorer because a hospital bankrupted your parents also has potential health implications in a country like ours. These unwise home births would be discouraged if hospitals would cease decreeing that VBACs or vaginal breech births are not "allowed" and threatening to get court orders to strap women down for unwanted surgeries.
I do think Dr. Amy is quick to attack anyone who criticizes her at all, but that is part of her style. I didn't read too much about the argument, but if I was on the receiving end of Dr. Amy's wrath over something so little I probably would have let it go.
The only "sloppiness" I saw from Jamie was in her not being able to reconstruct how the mortality figures of 2.06 and 1.61 per 1000 were derived. I admit in my post that I had trouble initially reconstructing them myself. So I'm not sure how "sloppy" that was.
Citation needed. Specifics matter.
As I almost certainly will do if she attacks me for this post; that is, unless she can demonstrate concretely that I'm definitely wrong about something. And unless, of course, I'm in a cranky mood when I see it. :-)
Part of the problem is that two different questions are being asked. The first is, "what is the added risk of homebirth per se?" Answering this question requires holding the risk of the pregnancy constant and just analyzing the effect of place of birth. The second question is, "what is the risk of homebirth as practiced?" This means determining the difference between what the risk of neonatal death at homebirth SHOULD be and the risk of neonatal death AS IT IS. If homebirth is safe, the risk of death should be similar to the risk of death of low-risk women in hospital birth. That's because safe homebirth requires risking out women with complications. The fact that high-risk women are still in the homebirth sample is part of the reason homebirth in the US is particularly dangerous. Taking them out of the sample, therefore, could be seen as artificially reducing the real risk of homebirth.
Sorry, but I don't buy it. Fair comparisons involve comparing groups as close to each other as possible. If you leave out VBAC, breech, gestational diabetes, etc. in one, you have to compare it to a group in which those are excluded as well. That's how we do it in the cancer world; I don't see any compelling reason it should be different in obstetrics.
"The only “sloppiness” I saw from Jamie was in her not being able to reconstruct how the mortality figures of 2.06 and 1.61 per 1000 were derived. I admit in my post that I had trouble initially reconstructing them myself."
MANA intentionally made these numbers hard to find. They set a trap for journalists and Jamie fell right in. Somehow this is seen as a blemish on Dr. Amy's credibility. Rather it should highlight to everyone how MANA tried to mislead anyone looking into these stats.
I have to say that staking your flag on comment moderation policies as the dividing line between being and not being a skeptic is pretty shaky. I would think that there were far more important dividing lines.
Especially since the "censoring debate" bit is obviously false. It's not like Dr Tuteur was prevented from airing her opinions on her own blog, which is, at minimum, what I would expect if she was actually being "censored". Indeed, it's not like everything she posted at GroundedParent was summarily removed by moderators, for that matter, including her presumably original comment which described Jamie's analysis as a hatchet job.
I saw this back when it first exploded, too, and wondered what the stink was about. After all, Jamie came to the same conclusions as Dr. Tuteur: home births have an apparent increase in risk over hospital births, but more study is needed because of the severe limitations of the study. Dr. Tuteur did make conclusions based on an inappropriate comparison of groups. Her response to the criticism was confusing for its level of outrage and personal attacks.
I followed this a little bit, but had a different interpretation. I had the feeling Jamie was being a bit disingenuous in her criticism. For example:
“First of all, can I first point out that it’s a 4x increase, not 5.5x (1.6/0.4 = 4). Even comparing the homebirth cohort that includes high-risk births (2.1 in 1000) to the low-risk only CDC cohort (which is not a fair comparison for obvious reasons) would only result in a 5.25x increase in mortality. I seriously have no idea how Dr. Tuteur came up with 5.5x or 450% increase in mortality from the numbers that she cited.
Ok ok ok, but even assuming that Dr. Tuteur screwed up some of the basic math here […]”
To me, this is unfair. She uses 0.4 as the low-risk, while Amy used 0.38, and then claims that 2.1/0.4 gives 5.25, while Amy’s calculation seemed to be 2.06/0.38 = 5.42. Yes, it’s not quite 5.5, but close enough that most people would recognize that Amy was rounding up (that question of whether that was a fair comparison, however, is a valid).
Then she says thing like:“it’s not clear that we can get enough accuracy to the 1.6 per 1000 number to even determine that it’s truly “bigger” than the 0.4 in 1000 number from the CDC.”, “It is just not clear to me that these numbers are coming from sources that are similar enough that they can be compared to determine relative risk.”, “due to the small overall population and the rarity of these conditions, there were not enough births presenting these conditions in the sample to say for sure.”, “A future study using a bigger sample and matched comparison group will have to be done to really understand the relative risk between home and hospital settings in high-risk births, but until a better study is done, it’s best to go with the best evidence we have now (however flawed) and assume that having a high-risk birth at home is a bad idea.”
Jamie directly attacks Amy’s credibility. She does admit she does not know the literature on this topic (neither do I, for that matter), but she makes claims about the validity of the comparison as if she had the knowledge to do so.
Jamie concludes by downplaying the increase in risk seen from Amy’s analysis of the MANA study (and contradicting her ”birth at home is a bad idea”): “For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth” and by attacking Amy’s credibility once again: “The […] review by Dr. Amy Tuteur was […] just a sloppy and unscientific attempt at calculating relative risk by using two completely non-comparable data sources in order to scare readers away from homebirths.”
Then, in response to the analysis by Orosz, Jamie make the following claims: “but I’m not even sure why we are at the point of comparing them when I’m not even yet convinced that the cohorts are similar enough to be compared.”
If fact, it should be obvious that both her articles are based on this kind of arguments. Jamie is clearly arguing from ignorance. Just because she does not know if the values are comparable, it does not mean they are not, and that no one could possibly know. She clearly does not know, yet makes apparently absolutely no attempt to find out form an independent expert. I don’t want to sound as if the question of the comparability of the groups is not important and worth debating, but when I read Orosz’s analysis, it seem to my non-expert eyes that she made every attempt to favor homebirth in her choice of groups, and still showed significant increases in risk for home birth. In fact, Jamie seems to stubbornly persist in her ignorance in spite of multiple calls from Amy and other to ask for expert and independent opinion on this topic.
Jamie then continues with: “I’m going to give my opinion here if only so everyone will stop making assumptions […] it seems as though there is either no increased risk or a very small increased risk to having a homebirth in a low-risk birth situation” and “Again, this is my personal opinion and based partially in data, partially on guessing and assumptions regarding data I don’t have or doesn’t exist, and partially based on my personal valuation.”, and concludes with “However, there is no reason to mislead on the real risks. If you are against homebirths and you think that any possibility of a risk is not worth taking, then argue that without resorting to inflating the numbers.”
To me, Jamie came across as biased and unable to challenge her assumptions. Jamie acknowledges that “[MANA] did mention that there were factors that could increase risk, but in my opinion did not give enough of a warning about the possible dangers of having a high-risk homebirth.”, but does not seem to understand that this is done on purpose. She asks not to “[resort] to inflating the numbers” (which is a strawman), but fails to realize that what Amy is trying to do is prevent MANA from deflating the number. MANA don’t appear to want women to know about the risks of homebirth. Again, this is not my field of research, but it is particularly telling to me that MANA chose to compare their data to nothing else. It seems logical to me that most researchers would have found the best possible comparison group, and then discussed the possible biases associated with this chose. Is this really unreasonable?
Again, maybe Amy's comparison of low risk birth in hospital to high risk at home is debatable, but Jamie's articles went beyond that. To me, in that process, she lost a great deal fo credibility for anything else of value should could have said.
In case anyone read this far, I apologize for the long comment.
Edouard Brière-Allard
I find it amazing that she asks if women can be sceptics.
Seriously, isn't that already a given? What makes her assume otherwise? Also her statements about censorship and her past history.
@Edouard
When I read it, the impression I got was that Jamie's primary criticism is that you can't make the conclusions that Dr. Tuteur when there are so many unknown variables that could make the comparison at best misleading.
Keep in mind, she agreed with Dr. Tuteur that homebirths did appear to have an increased risk and that the MANA study probably could not be generalized to the greater public.
As a follow up to my comment in #7, it turns out the link to the Consumer Considerations fact sheet is given correctly earlier in the OP.
Feel free to disregard #7!
And I used to agree with you, but have since changed my mind. (Just FYI, I run experiments in the social sciences, so I am not a total blowhard here.) The compelling difference between a cancer study and this one, is that in a cancer trial, the personnel (or at least their training) involved with control and treatment are the same. The accidental inclusion of more high-risk people in one group or the other is based on chance, and the only thing that varies is the treatment itself. In homebirth, the treatment of "homebirth" is a compounded: you are varying the place of birth, but also the training of the personnel in the treatment group. More importantly, the existence of high-risk people to the treatment group is not random, but directly related to the (lack of) training of the personnel in the treatment group: it is therefore PART OF the homebirth treatment. You can separate out the two parts of the treatment by looking at low-risk hospital vs. low-risk homebirth (place of birth treatment), and low-risk hospital vs. full-sample homebirth (combined place of birth and personnel treatment). You could probably even subtract one from the other to get the personnel treatment. But it is not inappropriate to look at the risk of "homebirth" as the combined risk of both place and personnel.
Comment #21 was in response to Orac, I apologize.
EBA (#17) did a much better job making the points I was trying to. Thanks so much!
Orac how do you want me to prove my claim of censorship? There are screen caps on the Facebook group for Dr. Amy, would you like me to email them to you?
Jane (#8) the difference is EU and Australia only have one type of midwife and they are university trained and work within the medical system. In the US we have CNMs and CMs, which are university trained (and attend about 20% ) of out of hospital birth, and CPMs and other lay midwives who attend the rest. The CPM credential only requires a high school diploma, 40 attended births (and you don't have to be the primary midwife for all of them) and passing a multiple choice test to be certified. Further this certification can mean little or nothing as there's varying though generally little oversight, no requirements for risking out or transferring patients and little accountability when they do fuck up. Most don't carry malpractice insurance. They don't have any hospital privileges and often don't work with physician or CNM oversight.
Many homebirth advocates claim homebirth midwives only take low risk patients and risk out patients once they stop being low risk. This is pproveably false simply by a quick look at MDC, midwifery today or Jan Tritten's Facebook pages or the homebirth board on babycenter. Women with GBS, for example, are often advised to shove a clove of garlic into their vagina to 'prevent' GBS exposure to the newborn.
The reason our data are so poor is because we have a second subpar class of midwives who attend homebirth.
I would be careful about prosecuting mothers for birth choices. Criminal law is a very heavy handed weapon, and should be used carefully for personal medical choices. As Orac points out, it's not clear the increase in risk here for low birth - while a powerful argument against choosing that choice and powerful justification for carefully regulating it - justifies classifying it as the negligence or recklessness necessary for a criminal trial.
The gender comment above is extremely troubling. And thanks for walking through this, Orac.
Well, whenever Dr. Amy is involved there will likely be vitriol! I think a lot of it this time was that Jaime's post was very sloppy and seemed to be implying Dr. Amy quoted something which didn't exist when really Jaime just hadn't looked very hard for it. There were also the politely worded corrections that were deleted and the refusal to fix any mistakes apart from a simple and obvious math error.
The statistics professor eliminated the code for congenital anomalies to get her higher number, but Dr. Amy did not. The reason Dr. Amy's numbers were so low were because she looked at only white women since there were so few black women in the MANA statistics and she chose certified nurse midwives on the basis that they would have a lower/more comparable risk profile since there were few risk factors in the MANA group. The numbers including OBs would include type I diabetes, morbidly obese mothers, a higher percentage of breech presentation, and many other high risk mothers who would not have had homebirths. She posted a video showing how to get her numbers (http://www.skepticalob.com/2014/02/calculating-neonatal-mortality-using…), though she must have done some math beyond that since the CDC wonder database won't allow the date range she be used to be looked at all in one piece.
Dr. Amy's numbers are not quite the right comparison group either since breech births and would almost certainly be risked out of CNM care and some other conditions that MANA midwives may not even test for. I understand why she did it though - she was making a point that MANA midwives keep saying breech is just a variation of normal and perfectly safe to deliver at home and gestational diabetes is no big deal and no real reason to test for it and inserting garlic in the vagina is an appropriate way to deal with the risk if GBS, so she's going to take them at their word and consider these all low risk and so compare them against hospital low risk. Which, it is a good point, and she said clearly what she was doing, but she should have made her point and talked about what the actual risk for truly low risk women might be and how each risk factor effects things.
The absolute risk of homebirth is still low, but each perinatal death is a tragedy, and much of the risk could be ameliorated by proper training and licensing of midwives which would allow them to be better integrated into the overall system. Also there is a big factor of honesty, which seems to be Dr. Amy's main point - how can MANA announce these numbers, which they have sat on for years, and claim they show homebirth is as safe as hospital birth? Also, then absolute risk for some situations such as breech birth is not at low, and MANA has known this for years, but still harped on about "variation of normal" and encouraged them to happen at home, How is that informed consent?
There are well respected "elder" midwives who do not believe in carrying medication to slow/stop hemorrhage - just stick some herbs or a bit of placenta under mom's tongue, and it will do just as well! There are those who discourage ultrasounds (might cause cancer... or autism!) and believe that as long as the umbilical cord is not cut, there is no reason to worry and rush to resuscitate a baby who hasn't taken a breath yet because they will still be getting oxygen through it. How many babies died or were brain damaged (another study showed homebirth babies were something like 16 times as likely to end up in the NICU getting cooling therapy to try to preserve brain function) because the midwife didn't realize the placenta was already detaching and not supplying oxygen? Absolute risk being low or not, there is just no excuse for that sort of incompetence.
I know Dr. Amy's stuff was a little confusing since she posted about in about a zillion posts in a short period of time, but if Jaime was going to take issue with her work, she really should have taken time to click on all of them and at least skim. Jaime's post was quite lazy and a bit insulting, and Dr. Amy is super touchy and likely to go off on people, so there you have it, drama.
Dr. Amy made a youtube video showing how she arrived at the 0.38 number: http://www.skepticalob.com/2014/02/calculating-neonatal-mortality-using…
Jane: I noticed that no one has responded to your question about studies in Europe concerning midwives. The population of midwives in Europe and the United States are not comfortable. The closest comparison to midwifes in Europe are probably certified nurse midwifes in the United States. However, homebirth thing is mostly the territory of certified professional midwives (whose minimum training requirement is a high school degree) and direct entry midwives who have no formal training whatsoever.
@Jane,
If really looked at the perinatal mortality rates of homebirths in Europe, especially UK and the Netherlands you'd need to reconsider your statement that they don't show an increased risk.
You also need to consider the fact that the United States does not have the strict licensing requirements or strict definitions of risk that European countries do. IE, in some US states it's legal for someone with just a high school education and some online courses to treat a VBAC twins pregnancy.
You state that 1/3 of women in some hospitals are subjected to a C-section. You should be aware that this includes planned, high risk, and repeat C-sections. The rate for an unplanned section is more like 1/5 in the US.
Now, I fiddled around with the CDC Wonder Database a while trying to see if I could replicate Dr. Amy’s number. I couldn’t.
What search terms and limitations were you using or do you think should be used? I like playing with CDCWonder database and could try to reconcile the numbers if you're interested.
Jane, before you get too excited about the wonders of midwives and home birth in the Dutch system consider the following article which shows higher neonatal mortality in low risk infants delivered by midwives versus high risk infants delivered by OBs.
Orac: When blogging on something another skeptic has written, if there's any confusion whatsoever about what you're reading, do you contact them and try and clarify this before you write your post? After going and reading all the posts around this issue it's certainly appears that Ms. Bernstein did not do this initially. And prior to her response Dr. Teuter, does not appear to have tried to make contact either. However, after having your post criticized as inaccurate and manipulated, I can see how one might respond less than "politely".
CDC Wonder Database results:
http://whatifsandfears.blogspot.com/2014/02/mana-study-comparing-mortal…
Hospital MD neonatal mortality rate = 0.62/1000
Hospital CNM neonatal mortality rate = 0.38/1000
As someone else linked, Amy Tuteur also made a video on her site to show exactly how she got the numbers.
Did you read the comments? Did you read the many people who listed multiple errors made by Jamie?
Not fair to compare high-risk homebirth to low-risk hospital birth? Not fair? It's more than fair. Homebirth midwives claim that they only take low-risk women. They claim that high-risk is just "a variation of normal". That's their selling point. So, not high-risk enough to take them and their money but too high-risk to be included in the stats? Having one's cake and eating it, too?
To me, this alone is the hardest of all arguments against homebirth midwives. How is pointing out their imcompetence and lies unfair?
I cannot believe Jamie Bernstein didn't know this. Everyone who took the time to read more than one of Dr Amy's posts knows it's her main beef with homebirth. For this, and the reasons others have posted, I call her work sloppy.
I've written it many times over Dr Amy's blog: you can't have it both ways. Either midwives are so incompetent that they cannot recognize high-risk when they see it, so they are guilty, or they are knowingly taking high-risk women (deceiving most of them that they are not high-risk but just experiencing "a variation of normal") and they are guilty.
Either way, I cannot see why we shouldn't accept midwives at their word and their very own PR: each woman they take is low-risk, so she should be included in the stats.
Cannot overstate this, but it isn't just an issue of absolute risk of this or that. Its an issue of preventable death. A baby dying is an agonizing thing to go through, but what is worse is when you know it could have easily been prevented. Midwives lie about their numbers. They will never say "its slightly more risky than hospital birth". They tell you its actually safer than giving birth in the hospital (or exactly as safe). Then there is the shameful issue of MANA making absolutely no recommendations based on their 'study' (a non random survey with a 30% reporting rate) even though it showed that the rates of death for breech/twins/vbac were totally unacceptable by anyones standard. They just don't care. This survey was the best possible scenario and it STILL shows an increase in death. That should be deeply concerning to anyone who is concerned about getting to the truth of the matter here. The real numbers are much worse, I'm sure.
I know, I know. I'm at work right now and haven't had a chance to look at it. It's really a fairly minor point, given that I came up with a number pretty close to hers after I fiddled around some more and excluded congenital malformations, as I discussed in my post.
I'll leave this comment here since it was ignored by Jamie and moderators over at GP (as were pretty much all of the comments that pointed out issues and/or Jamie's obvious errors).
Alli (comment on GP) said “I’ve been trying to think of how to explain why I didn’t and still don’t find Dr. Tuteur’s comparison misleading, and I think I finally put my finger on it–it’s really a comparison of home versus hospital *midwifery* care.”
Yes yes YES. Thank you for spelling it out better than I did.
Women choosing to have a high risk home birth is one thing…. but women unknowingly having high risk home births is another… women who *think* they are low risk. As I have said before, I can’t help but wonder if the pre-e and GDM moms in the MANA study knew ahead of time of their issues… specifically the pre-e and GDM moms who ended up losing their babies due to their high risk issues. Did they know? Were they screened? Did their midwives just miss or ignore or dismiss the red flags?
I watched on youtube a breech home birth… an ACCIDENTAL breech home birth. I was FLOORED! The mother had no clue and when the midwife found out the baby was breech, there was no discussion of risks, there was no talk of transfer…. nothing. Just the discovery of breech baby and then kept right at it. So much for informed consent! The shocking part is that it is really not shocking anymore. B/c THAT is home birth in our country. It is a lack of informed consent, lack of screening, lack of monitoring, lack of acknowledging the real risks in high risk situations.
Until there are changes made to home birth in our country to ensure that it is for TRULY low risk women only, then a woman has no idea what kind of midwife she is getting, no idea if she’ll be getting informed consent, no idea if she will be getting the truth about the importance of screening measures, no idea if she’ll be properly monitored, etc etc etc.
I wish I knew how many women have home births each year who think they are low risk but are actually high risk.
**
That was my GP comment. And I just want to add.... I just received an email this morning from a friend. Her friend was planning a home birth with midwives. This woman suffered a catastrophic outcome b/c her midwives lied about her screening results!! This woman DID take her screening measures to ensure she was low risk... and she WAS high risk. And had NO CLUE b/c her midwives didn't tell her the test results. This just happened in the last week.
This is home birth in America! A woman choosing home birth, thinking she is a good, low risk candidate, may have no idea her pregnancy is high risk by the time the birth rolls around. THIS is why comparing hospital midwife-attended births to all-risk midwife-attended home births is reasonable.
And just a side note... not all of the births in the hospital CNM group are low risk. Some hospital CNMs see certain types of high risk patients.
We can't easily directly compare home birth in the US to hospital birth, but we can compare the perinatal mortality rate for the US to home birth in Canada. Canadian perinatal mortality for home birth was 0.35/1000 in this study from 2009.
http://www.ncbi.nlm.nih.gov/pubmed/19720688
Canadian midwives with hospital privileges, significant education and appropriate risking out have excellent outcomes. Why isn't anyone asking why Canadian home birth is coming in with much better safety rates even compared to the low risk MANA cohort? I think it is fairly clear that American home birth is vastly less safe than home birth practiced in other countries.
"I know, I know. I’m at work right now and haven’t had a chance to look at it. It’s really a fairly minor point, given that I came up with a number pretty close to hers after I fiddled around some more and excluded congenital malformations, as I discussed in my post."
It's not a "minor point" though. Don't you see? You are calling out someone else's credibility by leading your readers to think that Amy Tuteur may have lied or manipulated or whatever to get those numbers b/c you (and Jamie) can't seem to figure out how Amy T got those numbers. Why didn't you just ask her?
Jamie's two posts on GP were very lazy and full of errors. THAT is what people - myself included - had issues with. She was making strawman arguments, twisting things around, etc... it seemed like she was trying very hard - pulling whatever stunts she needed to - to make Amy Tuteur and Brooke Orosz look sloppy/wrong. It was not skepticism.
The problem with all of this Grounded Parents debacle, is there just seemed to be a personal vendetta about Dr. Amy and in many ways further gives ammunition against what Dr. Amy discusses. Yes she can be over the top opinionated (but believe it or not I've been following her for 5 years (same amount of time I have been reading your blog) and have seen a softer side from her too), but you know what, when other non-CPM midwife studies come out it seems those rates are often similar to what Dr. Amy has posted. Perhaps the math is slightly off, biostatistics is not an easy subject and I'm sure even experts get things wrong from time to time.
You know what though, I have seen Dr. Amy make corrections, I have seen her take certain tone-related comments seriously and I have seen her drop certain contentious subjects all together (she had a post about parenting outside the standard nuclear family 5 years ago, one I didn't agree with and hasn't brought it up again). Yes, she's contentious, but she's consistent and pretty accurate overall.
I have also seen her time and time again stand up for the woo that has infiltrated Prenatal, birth and infant care, much of which is infuriating, sanctimonious, full of shaming, and can be extremely dangerous to the women and children. My brother and his wife had prenatal classes at one of the top science-based hospitals in Canada, and some of what he saw made his jaw drop at how woo-ey it was.
Grounded parents had some much material to work from when doing posts about homebirth, pregnancy and infant care, but they chose to publish an article bashing another skeptic. At the end when Elyse said that she's no longer anti-homebirth due to some of its activist (Dr. Amy), it was beyond infuriating to a mom who has seen more and more woo come into parenting practices since I had my own child 8 years ago. To me, Jamie and Elyse could have used Dr. Amy's comment section to call her out instead of a blog post that in the end had homebirth midwives promoting it.
I'm actually quite sick of the stupid dispute. Again, there is so much woo in the Natural Childbirth Community that can be addressed. Do I think it's okay for skeptics to disagree? Sure, but I suspect there is a lot more to this than just numbers. Needless to say out of the first few posts from Grounded Parents on the subject of birth I have been disappointed.
To Dorit's comment in #25: I don't think anybody, and certainly not Dr. Amy, has advocated for removing or prosecuting a mother's choice to have a home birth. The issue is whether a second, uneducated class of home birth midwives (not CNMs) should be allowed to charge quite a bit of money to attend homebirths in a professional capacity. All over the US, CPM and lay midwives avoid prosecution or any sort of penalty for presiding over the deaths of babies and mothers who would have lived if not for their incompetence. They usually have no insurance. If they want to charge money to provide midwifery services, then they should be held accountable for their outcomes the way any actual medical professional would. Right now, that is not the case.
What nonsense. (See, I can be like Dr. Amy when I want to be.)
I was simply pointing out that a full list of all the parameters is necessary for anyone to replicate such a search, and at the time I didn't know where to find that list. When I came close to her number on my own, I was satisfied that nothing obviously weird was going on and explicitly said so in my post. Did you bother to read that part?
So I missed that Dr. Amy had made that video. It was easy to do. Mea culpa. You're making the proverbial mountain out of a molehill.
ANH - Sorry, there's no justification for limiting the discussion of C-sections to "unplanned" C-sections. Some of the women who avoid OBGYNs do so because they are justifiably afraid of being told that they must have a C-section; those would be considered "planned". Others are justifiably afraid that they will be coerced to submit to electronic fetal monitoring, which has no apparent benefit but greatly increases the C-section rate. There are some hospitals where the C-section rate is far higher than one-third. That's not "necessary" by any standard.
The study cited by PrecipMom shows that home birth need not be dramatically more dangerous for low-risk babies than hospital birth - and may even be less dangerous when all the downstream consequences of excess interventions are considered. Those American midwives who are doing worse need to do better.
As to the counting or noncounting of deaths due to congenital anomalies: Such deaths may not be preventable no matter where delivery is. More, some parents may in fact not feel that perinatal death of a severely malformed fetus is a worse tragedy than a long NICU stay, torturous for the baby and psychologically and financially devastating for the family, followed by death or institutionalization. The goal of reducing the death rate to zero is neither possible nor necessarily beneficent.
@Doula Dani
I don't see Orac implying any such thing. They based their analysis on Dr. Tuteur's original article about the MANA study. That article did not state what criteria she used, nor did it include a link to the video she subsequently made showing what she did. It's great that she eventually explained how she got the numbers she got, but she should have either explained in the original post or added a link to the video. She didn't. Instead, she included an abbreviated description that was insufficient to duplicate her results.
As a layperson looking at the vairous posts, if I wanted to double check what people were saying and see how they arrived at the calculations and comparisons they did, that's a bit thing to leave out.
Dorit #25:
I would be careful about prosecuting mothers for birth choices. Criminal law is a very heavy handed weapon, and should be used carefully for personal medical choices.
I completely agree, and from what I've read at Dr Tuteur's blog, so ddoes she. But of course it's different from holding homebirth midwives accountable for malpractice.
@Orac
One thing I noted when this all blew up was that Jamie acknowledged that while she didn't know how Dr. Tuteur came up with her numbers, she did take them at face value as validly derived.
And also, there's a huge intersection between the home birth midwifery movement and the anti-vaxers. It's often the midwife who first convinces a mother not to vaccinate herself during pregnancy for flu or pertussis, and then not to give the baby Hep B or vitamin K (which I realize isn't a vaccine, but it is an injection) at birth. The real reason is that a lay midwife isn't allowed to give those injections in most states, so rather than send her client to a doctor, she convinces her that it's not necessary if you just eat enough kale. This is the same reason lay midwives tell clients to stick raw garlic in their vaginas instead of obtaining antibiotics for Group B Strep.
I would like to add comments regarding other topics addressed by Orac.
First, the insults flying in this debate. Orac said “So why all the vitriol from Dr. Amy? (Yes, it’s mostly coming from her.)”. Frankly, I think you are wrong. Jamie made it clear in her articles that she though Amy was either lying or incompetent (see previous quote or full article), and supplemented that with comments like this one (see comments, first article by Jamie): “I assumed you wouldn’t purposefully mislead. I apologize for making this clearly incorrect assumption.” Although Amy was attacking, I feel she was only responding in kind to what Jamie was saying. Not necessarily mature, but that’s her style. I would not expect her to start being nice when people insult her knowledge or credibility.
Second, for your claim that Amy made “unnecessary insinuation that some women can’t be skeptics because they’re too touchy-feely and concerned about not offending”, I think you are misinterpreting what Amy was trying to do. Here are some other quotes from that post:
“It’s hardly news that the skeptic community is dominated by men. Part of the reason is pure, old fashioned gender discrimination and harassment. Apparently some male skeptics feel threatened by women and want to frighten and harm them.”
“Women are not less logical than men. Rationalism is not the province of men alone. Women are perfectly capable of succeeding in the hard sciences and do so every day.”
“I’m beginning to wonder if there is a germ of truth to the claim that there are not more women in skepticism, because women are so anxious to avoid confrontation.”
“So can women be skeptics? Of course they can. They have the same ability to succeed in science as men, the same ability for rational thought as men, and the same inherent ability to give as good as they get in free-wheeling debate.”
I don’t see much wrong with this, or the rest of Amy’s post. It’s true that Amy did go on to insinuate that Skepchick in particular could be was one of those that was “so anxious to avoid confrontation”. I don’t even think Amy herself believes this, and I have not seen Jamie make tone arguments. I saw it as a way for Amy to try to get Jamie to respond intelligently to her criticism. It was my impression that Grounded Parents and Jamie were perfectly happy to let the matter drop and keep their arguments from ignorance intact. Amy, on the other hand, has a dog in this fight. She wants the risks of homebirth with lay midwives to be recognized so that women can make informed choices. It appears that she chose to attack Jamie’s credibility as a skeptic to get her to look at the issue and correct her mistakes (the issue of whether or not this tactic was necessary or useful is debatable).
Thirdy, you mention people of treating Jamie differently than Steven Novella because she is a woman. You write: “Moreover, one can’t help but note that Steven Novella came to the same conclusion that Jamie did long before I looked into this matter; yet I haven’t seen him criticized the way Jamie was.”
Here are Steven’s conclusion:
“The MANA data is legitimately concerning. Trying to whitewash such results paints MANA in a very bad light. If they wish to promote midwifery they need to be honest about and own those results, and explain why they believe homebirths are still a reasonable option.”
and Jamie’s conclusion:
“For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low. […] [MANA] did mention that there were factors that could increase risk, but in my opinion did not give enough of a warning about the possible dangers of having a high-risk homebirth.”
Steven and Jamie conclusion are different enough, in my opinion, to justify the different response from Amy. Steven said this data is troubling and demands accountability, while Jamie does not recognize the dishonesty of MANA and still thinks homebirth from lay midwives could be safe. That being said, I would not be surprised if some of the difference in treatment from the community at large (i.e. not Amy) could be attributed to sexism.
Again, sorry for the long post, but I felt the quotes were necessary.
Edouard Brière-Allard
PrecipMom:
As this OP and comment thread is about a blog scuffle between authors who self-identify as skeptics, specifically regarding analysis of the MANA study, I can't see that the Canadian/BC study is pertinent. (*)
That said, it certainly would be worth bringing up with MANA.
(*) To be clear, the study you linked to is specific to British Columbia and probably cannot be compared to other provinces; I believe someone upthread (or maybe it was someone on the GP thread?) may have already mentioned that provincial standards for midwifery vary.
I have been a regular follower of Dr. Amy's blog for a while, so I am familar with her arguments on the grounds of infant mortality. However, I've started to notice that she devotes very little time to discussing maternal mortality and maternal health and satisfaction outcomes. From the limited data I've encountered (from sources that I have no doubt may be biased) homebirth (or at the broadest, midwife-assisted birth) results in lower maternal mortality and greatest maternal satisfaction after the experience.
I can appreciate that Dr. Amy goes to great pains to emphasize that she supports women's rights and reproductive rights. However, it seems like she sometimes gets very close to the "do what's best for your unborn baby" line of argument that is so prevalent among repro-rights opponents.
The largest question I always toss about in my head is whether or not it is acceptable in some form for an expecting woman to prioritize her own experience as paramount during birth. Is the rather obvious increase in infant mortality an acceptable tradeoff to create an experience that will be more satisfying and enjoyable to the mother?
I'll also note that Jamie also pointed out some of the flaws and weaknesses of the MANA study.
"There are some hospitals where the C-section rate is far higher than one-third."
If anyone needs an example of the kind of clueless and biased reasoning that homebirth advocates so often indulge in, look no further than jane. Pointing to the rate of CS of this or that hospital without thinking that those can be first rate medical centers where high risk cases converge...
Todd and Orac:
Dr. Tuteur said in her post "the neonatal death rate for low risk white women at term from the years 2004-2009 is 0.38/1000"
Based on that, I would perform the following search:
White women
Singles (no twins or higher orders)
37 weeks and above
Birth weight of 2500 grams or more
Live birth through 27 days (the neonatal period)
Years 2004-2009
(a preterm and/or IUGR baby would not be low risk)
Which gives 0.38/1000 for the hospital CNM group - which is mostly low risk women.
I understand it wasn't spelled out exactly in that particular post by Dr. Tuteur, which is why I still don't understand why - if someone wants to write an analysis or criticism - why not be thorough and just ask the author how they got the numbers?
@Trixie 43: I was replying (belatedly, and without making that clear) to comment 1 - but now that you mention it, I may have misinterpreted the comment: It may have referred to prosecuting the midwife rather than the mother. I think your other points are well taken.
In re comment #45 by jane,
1. A woman who is afraid of C-section and tries to avoid it by seeking a non-medically trained midwife may be getting the option she desires, but may not be getting the medical care she needs. It is not valid to hide that critical difference.
2. Similarly, "excess" intervention is a medical judgement that should be made by medically trained personnel.
3. One major problem with your concluding paragraph
calling for allowing newborns with major congenital defects to die is that a non-medically trained midwife might not know what effective medical treatments are available. Given the already woo-filled nonsense suggested by non-medical midwives I have read just in the comments to this post (anti-vaccine, anti-vitamin K, anti-antibiotics, not revealing high risk test results), I would not want to allow a layperson to give life or death medical advice.
4. Furthermore, (yes, this last is a stretch) it would be fairly easy for an individual to claim that an infant's death was due to a treatable congenital abnormality rather than malpractice.
@Doula Dani
I agree that it would have been better for Jamie to do her due diligence and ask Dr. Tuteur how she got her number from WONDER, but it is still a fair criticism to say that Dr. Tuteur should have spelled out what she did in her original post. A layperson may guess what variables constitute low-risk, but they would, at best, be guessing at what Dr. Tuteur selected and could end up including or leaving out certain groups that should have been left out or included. It's a criticism we level at anti-vaxers regularly when they make some claim: show your work.
In re my comment #57, point 2, ideally the decision should be made by the parents, in consultation with medically trained personnel who have objectively laid out all of their options for medical intervention with clearly stated risks and benefits. I realize this is an ideal, but going 100% the opposite way into blind avoidance out of fear is just plain ignorant and dangerous.
@ Todd,
You are right that Dr. Amy should have put in an explanation or a link to other posts showing how she got the numbers, at least retroactively, once she realized people were confused. But leaving it out was an oversight, not a deliberate attempt to hide a faulty comparison. Jamie's accusation that Dr. Amy was being deliberately misleading is what people are upset about.
Todd,
I agree. It would have been much easier to understand and would have alleviated a lot of confusion if it were better spelled out in that particular post by Dr. Tuteur.
@yizz
Regarding the WONDER figures, Jamie did not suggest that Dr. Tuteur was being misleading. She took her at her word. The bit where she used the word "misleading" was in reference to how Dr. Tuteur added the numbers from the original study, and that's afternoting in the original post that "The stats she mentions (2.06 per 1000 risk of death for all births and 1.61 per 1000 risk of death for low-risk births) are not mentioned anywhere in the actual study, though that doesn’t mean they are not accurate." and that "those were numbers for what the paper deemed as the “low-risk” cohort. In your post you said the 2.1 in 1000 number was from the cohort including high-risk births."
The "misleading" comment was perhaps ill-advised, but I didn't read it as a serious accusation, in light of how Dr. Tuteur closed her response:
"...ideally the decision should be made by the parents, in consultation with medically trained personnel who have objectively laid out all of their options for medical intervention with clearly stated risks and benefits"
Ideally, parents who then ignored the advice of medically trained personnel and rejected medical intervention despite being advised of the increased risk, would be politely but firmly turned down by every midwife in their area.
EBA,
Thank you for taking the time to lay it out there so well. I hope everyone reads your comments.
Imagine for a moment that a bunch of chiropractors got together and formed a professional lobbying group to defend lax regulations on their profession. Then imagine that they had a survey (that they misleading called a study) about outcomes, a survey that was filled out after the fact on a totally voluntary basis. Only 30% filled out surveys and no explanation was given for the other 70%. Lets imagine that the survey still showed that there was an increase in danger to patients over getting a massage. Imagine the lobbying group published the numbers without any oversight or peer review from another group, and put it out with a press release that outright lies about the data.
....Then imagine that skeptics fell all over themselves bickering about if how so and so blogged about it was misleading or not instead of focusing on the fact that cherry picked data STILL shows an increase in danger, which could lead one to reasonably conclude that the real numbers are much worse.
Amy just wrote a response to this on her blog. Thought you might need this: http://youngsgifts.com/images/at_home/emergency/704-443064.jpg
Well, that's the difference between skeptics and quacks. We care about how the numbers are derived and want it to be done correctly. It matters to us.
Jane,
If you want to take issue with modern obstetrics you can do it with Dr. Amy on her blog. She's addressed these points, even if you don't like her answers.
Your argument amounts to absolving midwives of responsibility for their professional decisions. Hospital policies explain, in part, why there is demand for high risk deliveries. It does not explain or excuse midwives' willingness to perform them. How many of these midwives will say, "You can have a home birth, but a C-section in the hospital is safer, even if your first choice would be a hospital vaginal birth"? They don't. Professionals have a responsibility to recognize the limits of their competence even when patients demand more.
The reasons other countries have better results have been addressed by Dr. Amy. The midwives are better trained, integrated into the system, and don't perform high risk births.
Indeed. Dr. Amy's response was completely overwrought and far out of proportion to any perceived "offense," particularly the persistence of it over multiple posts. Then when she brought the whole issue in of "some" females (translation: Skepchicks) being unable to be good skeptics because they are too averse to confrontation, that topped it off.
I figured she would. I'm only surprised it took her a whole five or six hours. If I decide to respond right away, she'll respond again immediately. We've seen this pattern play out in this unfortunate kerfuffle. If I don't respond right away, she'll probably write a taunting post claiming I'm "afraid" of her or finding some other thing to attack over. So I'm in no hurry to respond because she can always bury me in posts; there's nothing to be gained by getting into a pissing match. Instead, I'll respond in my own time on my own schedule.
Hardly.
Jane
ANH – Sorry, there’s no justification for limiting the discussion of C-sections to “unplanned” C-sections. Some of the women who avoid OBGYNs do so because they are justifiably afraid of being told that they must have a C-section; those would be considered “planned”.
This is something I can comment. The wife of my best friend is an epidemiologist surveying the needs of C-Sections and she is responsible for a lot of epidemiological data (meta-analysis) which should affect the needs of C-Section because the data show that after a few years, pregnant woman don't always need a C-Section after having one for the first pregnancy.
http://www.ncbi.nlm.nih.gov/pubmed/?term=St%C3%A9phanie+Roberge
Alain
Of course, that's not what she did, at least not as explained in her very first post. Certainly she mentioned nothing of this. Let's go back to what she did say:
Nope. No mention of isolating place and personnel in her original post. She's still wrong, as far as I'm concerned. In fact, now that I think about it, she's even wronger. The Wonder database doesn't allow one to look up the six week mortality, which is what the MANA paper reported. So Dr. Amy compared four week mortalities (which the Wonder database does let one look up) to six week mortalities in the MANA study. It probably doesn't make a huge difference, but it's just another way these figures are not easily comparable.
This is particularly ironic in light of the amount of confrontation, flame wars, dealing with unsavoury behaviour, etc. that Skepchick and its affiliates have been through on matters pertaining specifically to feminism.
On the matter of comments policies, which Dr Tuteur specifically brought up, I would put forth Skeptical Science (*) as an inexact parallel: Skeptical Science has a stringent comments policy - in fact IMO it is far more stringent in several respects than Skepchick and a very active set of moderators who enforce it. (It's also an inexact parallel because, as far as I am aware, most of the Skeptical Science writing team do not self-identify as skeptics the way that, say, Orac, the Skepchicks, or members of JREF do.)
So if Skepchick is insufficiently skeptical because of the specifics of their comments policy, what of Skeptical Science?
Skepchick comment policy.
Skeptical Science comment policy.
(*) For those unfamiliar with the site, Skeptical Science discusses climate science, and has an extensive collection of self-styled "skeptic" arguments against the science that it refutes, with reference to the existing body of evidence. Skeptical Science updates its articles and publishes new content on the basis of new research on a regular basis.
D'oh, missed a closing hyphen.
Is there any consideration for the added risk of transporting a laboring mother from wherever she is (home) to the hospital? It would seem that there's an occasional baby born in traffic, plus inevitable traffic accident related injury and death.
Orac, I’ve been reading your posts on this blog (as well as on the other one) for a little while now, and I have to say that your response on this issue really surprises me.
Obviously, I have my own biases on this topic, but I really find it hard to believe that, as safer midwifery Utah (#65) alluded to, you would be having the same discourse if we had been talking about chiropractics, anti-vaccine advocates or cancer quacks.
In the comments, Orca said: “It probably doesn’t make a huge difference, but it’s just another way these figures are not easily comparable.”
Orac, I’m not your boss, and you can do whatever you want with your free time, but for crying out loud, you and Jamie should both stop arguing from ignorance and ask an OB or two if they think Amy’s analysis is as sound as it could be, given the limited data from the MANA study. In the mean time, I’ll stick with the OB’s opinion, thank you very much.
And just to be clear, I realize that your analysis of the data shows a risk. I only disagree with the fact that Jamie’s articles, and then yours, give the impression of dismissing the study as if it has no value, which is the impression I got when I read Jamie’s post (“neonatal mortality rate of having a homebirth [with a lay midwife] is either negligible or slightly higher than that of a hospital birth”). Sure, it’s not perfect, but when quacks publish a study that shows a product is unsafe, that last thing I expect is Orac comforting them by saying it may not be that dangerous as they showed it to be.
Edouard Brière-Allard
The Wonder database doesn’t allow one to look up the six week mortality, which is what the MANA paper reported.
True, but that rather supposes a massive death rate at the ages of 28 days-6 weeks. I'm not particularly familiar with pediatrics, but that seems fairly unlikely.
FWIW, examination of the CDC wonder database for 2007-10 using very loose criteria for "low risk" (mother's age 20-44, GA >37 weeks, mother's education at least HS, at least some prenatal care, weight at birth >2500 grams), and death at age 0-27 days gives a rate of 0.52 for doctor in hospital and 1.04 for other midwife out of hospital. (Changing the criteria to 39-42+ weeks makes the mortality 0.45 for doctor/in hospital, 1.05 for other midwife/out of hospital.) This is "only" a two fold increase, but it does make the point that it's extremely easy to demonstrate that survival is poorer for infants born in home birth.
Orac you said " The Wonder database doesn’t allow one to look up the six week mortality, which is what the MANA paper reported. "
No, the MANA paper did not report mortality rates up to six weeks. They reported intrapartum mortality and neonatal mortality. Neonatal mortality rate is live birth through first 27 days. They broke it up into early neonatal and late neonatal and also gave total.
To quote the MANA study:
"The rate of early neonatal death (death occurring after a live birth, but before 7 completed days of life) was 0.88 per 1000; and the rate of late neonatal death (death occurring at 7 to 27 completed days of life) was 0.41 per 1000. When lethal congenital anomaly-related deaths were excluded (n = 0 intrapartum, n = 8 early neonatal, n = 1 late neonatal), the rates of intrapartum death, early neonatal death, and late neonatal death were 1.30 per 1000 (n = 22), 0.41 per 1000 (n = 7), and 0.35 per 1000 (n = 6), respectively"
And total neonatal is in the discussion of the study:
" Our combined early and late neonatal death rates, or total neonatal death rate, of 0.77 per 1000..."
#27 "Dr. Amy’s numbers are not quite the right comparison group either since breech births and would almost certainly be risked out of CNM care and some other conditions that MANA midwives may not even test for."
There are CNMs who will do breech.
Jane, I'm in Ontario, and I delivered with RMs. Trained midwives, integrated into the hospital system. Guess what? They risked me out of my planned homebirth when I went postdates with a large OP baby. They told me to prepare for the possibility of a section since she was badly positioned and I have a narrow, android pelvis. That's good, honest, informed care. For what it's worth (nothing, to my way of thinking) it was a vaginal delivery. It really didn't matter in the end, so long as we were both healthy and safe.
Adam (#76) - the MANA study was for planned home births only, no accidents and it took into account transfers to hospital. However, certain clients who transferred did not have outcomes included (for example, several of the breech births that transferred during labor have an unknown outcome).
Knock out congenital malformations and otherwise keep the parameters as above and the neonatal mortality ages 0-28 days is 0.25 for MD in hospital, 0.77 for other midwife, out of hospital. Now we're getting up over 3x the risk. For delivery by CNM midwife (a closer approximation of true low risk), the rate is 0.16/1000, 4.8 times the risk.
Jane #45 "There are some hospitals where the C-section rate is far higher than one-third. That’s not “necessary” by any standard."
Which hospitals? Which specific cases were not necessary and how are you making that judgment?
A tiny comment on the C-section rate -- I would guess that it's gone up in part because of lack of training of younger OBs to deal with complicated deliveries vaginally, amplified by fear of litigation if a vaginal delivery doesn't go well.
My wife is an in-hospital CNM; at one point she was delivering a baby that turned out to be an undiagnosed breech. Here was this little butt hanging out and tiny penis flapping comically in the breeze -- very fortunately, one of the old, extremely skillful OBs was right down the hall, stepped in right away, and masterfully delivered a healthy little boy.
Very few OBs have that kind of training any more, I bet.
As to the counting or noncounting of deaths due to congenital anomalies: Such deaths may not be preventable no matter where delivery is.
Really? NO congenital anomaly can be treated? I guess I must be dead then, since I have a PFO. Funny, I always thought death would be...quieter.
Not all CA are fatal. Quite a number of anomalies can be treated. Others (like mine, in fact) don't require treatment. However, those that are both treatable and require treatment can not be treated at home. A baby born at home with transposition of the great vessels will die. One born in the hospital may survive.
To clarify my comment above, I'm talking about risks associated with hospital birth, not OOH. The 'getting there' part is relevant, since you don't have to get there if you're at home and planning a home birth. There's gotta be some risk there.
There are some hospitals where the C-section rate is far higher than one-third. That’s not “necessary” by any standard.
So you're suggesting that there be a quota and if the quota is reached, no more c-sections, because they're clearly unnecessary? Which c-sections are "unnecessary" and how do you know?
Hmm. "Kerfuffle" (instead of argument or controversy), "overwrought" (did you mean over-the-top?)... Orac, maybe you should work on the language you use when referring to women, before taking to task Dr. Tuteur for her polemical tone.
Oh, and talking about COI, maybe it should be mentioned that at least one of the Grounded Parents writers had one in this case, both with homebirth and Dr. Tuteur. She used on her blog, as an example of bad midwifery and deceptive marketing, a post by Chris Breechen recounting the homebirth of his partner. All that before Jamie decided to comment on Dr.Amy's analysis of the MANA survey, not on the survey itself. It's... interesting.
I've had three home births--results now aged 40, 36, and 28. Come and get me Mu.
I know Jamie too, and find her a noisy, irritating, non-stop chatterbox.
#84, "Very few OBs have that kind of training any more, I bet." -- and why do you think that is? The Term Breech Trial pretty much says it all. http://www.ncbi.nlm.nih.gov/pubmed/11052579
It's not just fear of litigation, it's fear of death.
Adam (#86)
"To clarify my comment above, I’m talking about risks associated with hospital birth, not OOH. The ‘getting there’ part is relevant, since you don’t have to get there if you’re at home and planning a home birth. There’s gotta be some risk there."
There are certainly risks when births happen accidentally that are intended to be in the hospital. Same risks apply to planned home births, though. A home birth midwife does not come at the first sign of labor. They typically wait until labor is well established. In which case, a mother who has a precipitous birth may end up at home unattended, just as if she planned a hospital birth.
Just anecdote but I know several women who planned home births whose midwives did not make it in time - b/c the labor was too fast, because the midwife assumed the labor would take longer (especially for first time moms who end up randomly having a fast labor), because the midwife was at another birth and didn't have a back-up midwife to send, etc.
We’re comparing apples and oranges in that there was no control group for the MANA study, and it’s always problematic to compare what is in essence such a highly self-selected group with population-based statistics. We have no idea if the MANA group was representative of women who choose home births, because it’s a group of women who not only chose home birth (less than 1% of pregnancies) but were also willing to sign the informed consent form to be in the study.
A couple of points on these issues.
1. According to the article, 95% of women approached signed informed consent. So they're likely typical of the population of women eligible for the study.
2. Midwife participation was voluntary. As far as I can tell, any given midwife did not have to report every pregnancy outcome. She could choose not to report women who had poor outcomes, for example.
I don't see any way that the population who participated and whose outcomes were recorded could be any higher risk than average.
@ # 45 jane:
"ANH – Sorry, there’s no justification for limiting the discussion of C-sections to “unplanned” C-sections. Some of the women who avoid OBGYNs do so because they are justifiably afraid of being told that they must have a C-section; those would be considered “planned”. Others are justifiably afraid that they will be coerced to submit to electronic fetal monitoring, which has no apparent benefit but greatly increases the C-section rate. There are some hospitals where the C-section rate is far higher than one-third. That’s not “necessary” by any standard."
Good grief jane. Must you always pollute Respectful Insolence threads with your uninformed, ignorant opinions about subjects you know nothing about? What do you have against obstetricians and licensed nurse-midwifes and the prenatal care they provide to pregnant women? Do those lay midwifes monitor expectant womens' general health? Do they test these women for the presence of Rh incompatability, hepatitis B carrier status, the HIV virus and other STDs? Do they do vaginal and rectal swabs at ~ 37 weeks gestation, to test for the presence of GBS and are they prepared to set up an IV antibiotic during the final stage of labor through delivery? Are these unlicensed lay midwives providing post-exposure hepatitis B vaccine/HBIG to prevent vertical transmission of the virus from a carrier mother to her child? Do these unlicensed lay midwives instill ophthalmic antibiotics in infant's eyes and do they administer Vitamin K shots to infants to prevent intracranial bleeds?
How about maternal gestational diabetes testing and maternal monitoring for the signs of the onset of preeclapsia?
Do these unlicensed midwives send infants blood to State labs to test for the multiple genetic diseases...many of which are preventable with special formulas or medication?
http://www.wadsworth.org/newborn/babhealth.htm
What do you have against electronic monitoring which can diagnose fetal distress?
"The study cited by PrecipMom shows that home birth need not be dramatically more dangerous for low-risk babies than hospital birth – and may even be less dangerous when all the downstream consequences of excess interventions are considered. Those American midwives who are doing worse need to do better."
That's small comfort to women who made the foolish decision to entrust their prenatal care to an ignorant unlicensed lay midwife. That's no comfort to the maimed and dead babies, that lay midwives left in their wake.
"As to the counting or noncounting of deaths due to congenital anomalies: Such deaths may not be preventable no matter where delivery is. More, some parents may in fact not feel that perinatal death of a severely malformed fetus is a worse tragedy than a long NICU stay, torturous for the baby and psychologically and financially devastating for the family, followed by death or institutionalization. The goal of reducing the death rate to zero is neither possible nor necessarily beneficent."
How about the malformed babies whose skulls were crushed or who suffered anoxia because of the amateur practice of lay midwifes?
Gee, you managed to solve the problem of providing services and resources for infants, born less than perfect. Thanks for your assistance with this societal problem.
Cripes, you and your ilk who think that "natural home birth is better" with unlicensed lay midwifes in attendance, disgust me.
Yes, the authors of the MANA study state that they aren't certain every midwife who participated entered info for each of their clients.
An interesting read from a midwife who participated in this very MANA study:
http://navelgazingmidwife.squarespace.com/navelgazing-midwife-blog/2014…
"The study says they enrolled the clients before they knew the outcome of the births, but I beg to differ. They may do that now, but back when I was doing them (2004-2009), we didn’t even fill out the paperwork until the woman was past six weeks postpartum."
"I am sure that midwives with a bad outcome just didn’t finish that woman’s stats. It would have been encouraged in the culture. So that so many did send in negative outcomes lets us know how bad the perinatal mortality and morbidity rate really was. "
I'll quote Irene up there:
"Hmm. “Kerfuffle” (instead of argument or controversy), “overwrought” (did you mean over-the-top?)… Orac, maybe you should work on the language you use when referring to women, before taking to task Dr. Tuteur for her polemical tone."
I do not have any particular bone in the contention, as I am neither from the US nor plannig children. I am, however, a female, part of the 50% of the World that doesn't have a penis, and this kind of language is very, very offensive to me.
I see that it's time for simply recycling stuff from Tuteur's axe-grinding and the lapping up of it from the commentariat.
Narad, I can assure you it is not. While it is true that she had pointed it out, it also happen to be true.
Pray, tell me why when Orac debates Mike Adams it is an "argument" and when he debates Tuteur it is a "Kerfuffle"?
I get you are a man, so it may not be something you have a lot of first hand experience in, but for women it is a true problem to be taken seriously. When women talks about "women's stuff" (childbirth, problems related to genitals, problem related to menopauses) in any way that is not woo-filled, then twice as much.
For a woman, this is the same as Orac talking about, say, something Neil deGrasse Tyson had said he disagree with and claiming:
"Well, that Negro said..."
Get the point now?
Oh, please.
I use the word "kerfuffle" all the time about all sorts of dustups, and have been doing so for years. In fact, I sometimes think I rely on the word too much, that it's too easy a crutch to describe an argument. Indeed, I've often thought that if anyone wants to do a parody of my writing style using the word "kerfuffle" several times would be mandatory. Just type the word "kerfuffle" into the search box and find how many times I've used it. (Hint: It's a lot.)
Ditto the word "overwrought," although admittedly I use this word less frequently. Still, for example, here I am, calling a Mike Adams' rant "overwrought"—and appropriately so:
http://scienceblogs.com/insolence/2013/10/11/the-court-intervenes-to-sa…
Orac, I also use words in normal speech that I wouldn't use when talking about particular minorities or such (as I am not a native English speaker, I can't give examples in English, though I could in Italian). In some case being PC is wrong. In some other it is not.
This is one of the second case.
This kind of use of language is insensitive and hurt your point. It would help if you could make clear that the relative sexes of the person in the discussion have no point in your talking, because from your writing, it is not clear at all.
I seem too sensitive? Perhaps. On the other side, I am actually a woman and I know how it is.
Orac didn't want to get into the second post of Jamie's, when she tried to critique the analysis by stats professor Brooke Orosz. So I'll do quickly:
Jamie thinks io9 was crazy for saying it was a "group of midwives" who wrote the MANA study b/c only one was a midwife and then said she wouldn't link to the authors to protect their privacy.
(3 of the 6 authors of the MANA study are midwives, 5 of the 6 are a part of the Midwives Alliance and the 6th one is a home birth mom. Yeah, the io9 author was sooooo far off.....)
Then Jamie made a bunch of strawman arguments.
The end.
So, I don't have a dog in this fight. I read the Grounded Parents article first and then followed the links to Dr. Amy's OP, which was my first introduction to her.
She's bombastic and hot headed. I also am not particularly bothered by her style though. She's upfront about it, and my understanding is she's a professional blogging about her specialty in a no-holds-heres-how-I-REALLY-feel kind of way.
Here's the thing though. I am not at all surprised this escalated. I'm honestly unclear why anyone is. Dr. Amy is a grouchy and touchy Grizzly bear. Jamie Bernstein poked her with a stick. And not a neutral stick. She poked her with the Stick of Personal Attack. I do not see how anyone can see her piece as just a neutral analysis of the numbers. It was not. There was a neutral analysis of the numbers IN the piece, ALONG with some personal commentary about Teutur.
Her characterization of Teutur's thesis alone was antagonistic. She summed it up as a kind of "OMG" comment, which is a pretty nasty way to trivialize someone's piece. And while she apparently agrees with the larger analysis that Teutur was getting at... she didn't use that kind of demeaning language regarding the Mana people.
Bernstein writes with a very different style than Dr. Amy, but she did not at all come across as a dispassionate journalist (I'm guessing this is how she wants to be perceived?). With no previous knowledge of the topic, Dr. Amy, or Bernstein I finished Jamie's piece wondering why the harshest language was used on the skeptic who made math errors but the Midewifery Group that was spinning it's numbers to it's own advantage was barely given a verbal slap.
In particular the equivocating about being unable to find the source of a quote, when an email to Teutur would have inevitably turned it up was particularly lame. That alone sings loud and clear that the writer was going into this with the intent to publicly take someone down, not understand how she came to her conclusions.
And Bernstein's response to the initial criticism of how she treated the quote issue: "It wasn't worth my time to go looking". This earned an /eyeroll from me. If she wants me to take her seriously as a writer, that excuse isn't going to cut it. Either verify the quote or don't bring it up.
I could pull apart both of Bernstein's posts for all the things I found problematic, but it's too much for a comment's section, and much has been covered earlier in the thread.
So Orac, I say with all kindness, I don't know what your previous experience is with either of these two. You probably have more insight that gives you a different perspective. However speaking as an outsider to both of these women I feel like there is bad behavior on both sides. BUT, Dr. Amy's bombastic style is up front. You know what she really thinks and you are free to disagree.
Jamie Bernstein's writing was something I found more irritating, given there was a level of underhanded insinuation I find... distasteful. She seems to be trying to pass as a neutral party while simultaneously sneaking in judgment and opinion of Teutur. I frankly would have found it all far less offensive if she had just been upfront and titled the piece "Dr. Amy is Wrong and Here's Why". Or at the very least admitted in the piece that what she was really doing was an analysis of Teuter's blog post and coming at it head on.
Well, so is my style, but not nearly as nasty and bombastic as Dr. Amy, at least not any more. It might have been more so in the past, but I've toned it down over the years. I know, I know. Some of you will find that hard to believe, given my cuddly nature, but if you doubt me go back and read some of my posts from 2005 through 2008 or so, and you'll see what I mean. In particular, look up some of my old takedowns of Vox Day or Robert F. Kennedy, Jr. The writing style sometimes surprises even me when I go back and read them—and I'm the one who wrote them.
That being said, I thought what I just did was to disagree. And, seriously. I wasn't anywhere near as nasty as Amy has been in this kerfuffle. :-)
Hey, T., how come I don't see you in the Skepchick comments with these same points when they refer to an internal debate as a "kerfuffle?"
http://skepchick.org/2014/02/disabled-write-for-us/
If English is not your first language, I could see how you don't realize that "kerfuffle" does not have any gendered connotations, unlike something like "hysteria"
Indeed. Quite literally, no one has ever, to the best of my memory, ever complained about my frequent use of the word "kerfuffle." It definitely has no gendered connotation that I've ever heard of and is such a wonderfully expressive word, too, which is probably why I use it too much. As for "overwrought," I can sort of see a touch of gender association; so I'll try to be more careful about my use of the word in the future. But "kerfuffle"? Forget it. I'm going to continue to use the word as I see fit, and if T. is offended, I really don't care.
I am fairly certain that MANA used the 6-week number so that they could use the excuse that you can't compare their numbers to the CDC data when it turned out their numbers were so much higher.
This post is really disappointing. Bernstein's posts were crap, why she is getting all these apologist posts in response is beyond me. She did a crap job and the response is really "Well Dr Amy (forget MANA) didn't spell things out clearly enough for her poor soggy brain!" Really? If you are going to take someone to task you should be thorough, correct, and prepared for their response. She was none of these things, and has no business being defended on GP or here. I would really expect more from this site, but there is clearly bad blood between the two of you, so it is what it is. Silly women and their kerfuffles. Thank goodness a man finally stepped in to set the record straight...or something.
Also, the issues with comments on blogs and the discussion of how much or little moderation is in a lot of ways it's own topic. Again I have a lot of respect for Orac so I'm willing to allow that there is a lot of back history with what Tuteur may have said regarding comment policy in the past that he doesn't want to get into (and I really don't think he should). But the evidence presented doesn't really make her seem hypocritical to me.
All I've gathered so far is she felt like comments on SBM were not moderated enough. And she feels like Skepchick is moderating unfairly and squelching debate and contrary opinion. It's not like moderation is an all or nothing proposal, so I don't actually see the contradiction between past and present views here.
That said I don't agree with her feeling that this is some sort of gendered issue where women can't handle debates. I commented on her blog already that I see this more as a part of the larger issue that internet culture is struggling with right now about moderation, comments, whether they are needed, not needed, and in what context.
Basically this it's an internet thing. Not a gender issue.
@lilady
I just wanted to thank you for your response to Jane - it was excellent. :)
Gold star (and/or Glass Onion) for Orac for the Beatles reference!
Everyone is aware that Dr Amy's own blog is completely unmoderated, yes? Bringing up that she had a problem with SBM's moderation policy and not actually explaining what that problem was, leaving readers to draw their own conclusions? Why would one do that?
Just type the word “kerfuffle” into the search box and find how many times I’ve used it.
As far as I can tell, you've used "kefluffle" frequently in posts but a total of twice in titles of posts.
@Lumen
"Jamie Bernstein’s writing was something I found more irritating, given there was a level of underhanded insinuation I find… distasteful. She seems to be trying to pass as a neutral party while simultaneously sneaking in judgment and opinion of Teutur. I frankly would have found it all far less offensive if she had just been upfront and titled the piece “Dr. Amy is Wrong and Here’s Why”. Or at the very least admitted in the piece that what she was really doing was an analysis of Teuter’s blog post and coming at it head on."
That is an insightful analysis. In fact, one of the things I like about Orac (here and his other locale) is how he is similarly upfront about where he stands, like it or not. (I like spunk and yes, even some snark.) But I agree with your impression of Jamie's piece, that's how I felt after reading it as well.
I pointed out two comments, one of which NoLongerCrunching erroneously thought was so darn clever that it needed to be cross-posted and the other of which was tone trolling directly imported by Irène with the ever-promising preface of "Hmm."
It's recycling.
I got the point originally, and it wasn't anywhere as dumb as this bit of taffy pulling. Let's go to the original rather than your attempt to add a layer of long-simmering, profound hegemonic importance to the term:
"Just as an aside, why do men with substantive disagreements have principled arguments, but women have 'kerfluffles' [sic]?"
Do they? This isn't exactly a common word, at least on this side of the pond. Read literally, the statement verges on the senseless.
The objection boils down to that, in Dr. Tuteur's view, the dispute is not being taken seriously enough, dammit! Given that it is plainly of towering import, the only possible explanation is sexism. Just as the only possible explantion for Orac's post is because he's been lying in wait for an opportunity to repeat the Night of the Long Knives.
As it happens, when two people who agree that there's a significant effect instead decide to declare BLOGWAR! over the tone of a dispute about assessing its magnitude and it doesn't amount to a dustup, I'd say 'kerfuffle' is quite accurate. (I would have added 'spat' to the Ngram plot, but it dwarfs the other two terms.)
So what? As I said, I use the word a lot. Seriously, this "kerfuffle" complaint is getting really silly. It's almost amused/annoyed me enough that I am tempted to try to use the word more for a while, until my readers cry, "Stop! Stop! Please stop!" Or until they stop reading. Whichever comes first. Maybe I'll include it in the title of every post for the next week—or try to start every paragraph with a sentence using it.
Don't worry, I wouldn't do that (probably), as I value good writing far more than I enjoy being pissy. :-)
No.
"The sticking point was the lack of a moderation policy. Every [SBM] comment thread spun out of control because certain people (almost all of whom came from [my site]) were free to post garbage that they could never get away with on [my] site.
"Interestingly, I rarely remove comments here (can't remember the last time I did) and I almost never ban people, yet people are able to control their behavior because they know it could happen."
Anyway, why would you suppose that "everyone" here would be aware of Dr. Tuteur's moderation policy? The very first sentence of the post makes clear that obstetrics is an infrequent topic.
I have to say I am VERY disappointed in this piece. Orac, you would NEVER accept this kind of shoddy work from others. Not going to the source, non sequiturs regarding the person, cherry-picking quotes that are favorable to Bernstein/unfavorable to Tutueur's arguments.
For example, the whole 1.6 vs. 2.06/1000 rate. Tuteur went into detail in subsequent posts-- remember she publishes every day-- on the numbers and why she felt they were valid comparisons. You didn't even bother to check with her OR her subsequent posts before you jumped on the Bernstein bandwagon. (EBA, Lumen, and DoulaDani listed other examples) Is that fair? Is that thorough? Is that "skeptical"?
Skeptics give lip service to reason and countering bias, but given the right circumstances (in this case, a friend being excoriated by someone you don't care for) even the great Orac is just looking to dig in and confirm his presuppositions and place them under the auspices of Almighty Science[TM]. Sad... though not unexpected.
Actually, I did check Dr. Amy's subsequent posts. (And, yes, Amy, I know you're following the comments here.) I was unimpressed; they were basically the same sorts of reasons I've already disposed of earlier in the comments. My post was getting too long, anyway, even by Orac standards. Maybe I'll revisit the issue next week. Or not.
I do, however, like to be fair. Perhaps you could point me in the direction of some Dr. Amy quotes that make her look better on this issue. I had a hard time finding them, even though I agreed that the MANA study showed alarmingly high neonatal mortality rates.
Let me put my COI out first. I trained as a certified nurse-midwife, and practiced as one for 5 years.
Also - I really dislike Dr Amy. She doesn't know or understand anything about CNMs, except that they are all bad, only OB/Gyns should care for pregnant women. I had several run-ins with her years ago, when she blatantly mis-represented what CNMs are taught, and she both refused to recant or apologize. So I won't read her writing any more.
As far as the MANA study...it's not well done. I heard about it years ago, from CNM friends (home birth midwives) who were asked to participate and who declined.
I have said before and I'll say it again - I understand why OBs practice as they do. I understand why many women don't want to go to the hospital to have a baby. Personally, I think the ideal solution is a birth center in or on a hospital grounds - near enough for most emergencies, far enough that birth is not treated as a disease.
And don't lecture me about OB emergencies. I've seen many in my 20+ years working...including a maternal death, several near-maternal deaths, neonatal deaths (including 1 SIDS death in the newborn nursery) and hospital-caused deaths and injuries. Stuff happens. Life happens. Nothing is 100% safe. And all we can do, as medical personnel is educate, encourage the best choice for the person, and hope they make a decision that leads to the best outcome.
Why's that?
So what?
Of all the comments I've made on this post, that's the one that catches your eye? I've written several comments with a lot more content re the actual issue (i.e. the accuracy or lack thereof of Bernstein's and Tuteur's analyses as well as the original paper) and a verification of your use of "kerfluffle" is what makes you respond?
I value good writing far more than I enjoy being pissy.
Well, you're not really a bad writer, for a surgeon, overuse of certain words or not.
(#118) I've actually seen Dr Amy advocate the exact same position you've stated. So far as I've seen, she doesn't have much issue with CNMs or CMs, but with CPMs. Perhaps it's a somewhat recent development, nonetheless she has advocated adopting a homebirth and midwifery system similar to Canada's.
She doesn’t know or understand anything about CNMs, except that they are all bad, only OB/Gyns should care for pregnant women.
Actually, it's my impression that she really dislikes CPMs but is fine with CNMs who, after all, have standards of care and real training. She's been pretty rude about specific CNMs, but she's also been pretty rude about specific OBs.
birth is not treated as a disease
I've never quite known what people mean by saying things like this. Birth is a dangerous abnormal physiologic state. It can and does cause short and long term disability and death. It may not be a "disease" per se, but neither is elective surgery and no one is advocating home liposuction. Er, I hope.
Orac, here's the thing. How do you think many women get their first introduction to anti-vaccination ideas? Through their home birth midwives and doulas, is how. Megan Sandlin, who recently wrote the Voices for Vaccines essay on leaving behind the anti-vax world, has written that it was her home birth midwife who encouraged her not to vaccinate and to "do her research". Even if you don't care much about obstetrics, you should care about that.
Christy Collins, the Nevada home birth midwife who crowd sourced medical advice from Midwifery Today's Facebook page, and ended up killing the baby, is anti-vax. They almost all are. This is the same movement of woomeisters and dangerous idiots that you fight against every day. In some ways, they may be more dangerous, because in 2014 in the US, you're probably more likely to have a dead child from choosing a home birth than you are from choosing not to vaccinate.
Completely agree, Trixie (#123).
One of the very first handouts I got from my home birth midwife was an anti-vaccine article. I still have it, in a pile with all the other handouts I got from her. She was my prenatal yoga teacher and gave handouts at every class to everyone.
There are so many good points here in these comments that I hope Orac is going to address. I keep checking back to see. I hope he won't just ignore all of the comments stating valid concerns like Ground Parents and Jamie did.
Referring to #68, I am glad that you care about how the numbers are derived but I think you are mischaracterising quacks. They care about how the numbers are derived when they think there is some real or imagined "bias". Thing is you got similar numbers, so your beef appears not to be with Dr Amy's numbers. So I'm trying to figure out what the issue is. Is it her tone?
What is your position on the paper released by MANA? Do you think their conclusions match their data? How would someone like yourself go about finding that out?
I'm with MI Dawn about the delivery suite; homelike, but not at home and not in a distant free-standing birthing center. Some easy births turn out to be not-so-easy and I would want to be just down the hall within the confines of a hospital setting, where the full complement of staff, equipment, blood bank and ORs are located, to give me and my infant the best chances for healthy outcomes.
Everyone could have just handled all this in two simple sentences: "This was not a study. It was a survey with a low response rate and no objective way to verify the data."
The end. No need for anything else.
#118
It's not a study.
"Stuff happens, life happens, nothing is 100% safe"...love it when this gets trotted out to rationalize one's beliefs. Life is inherently unsafe, ergo, I'll just drive drunk/smoke cigarettes/give birth with untrained, unqualified practitioners at home.
You've seen many OB emergencies? So did my Mum, who delivered babies from 1963 to 2003. That's a lot of babies. She can count the term neonates with no congenital abnormalities who died intrapartum on one hand. Read MANA's data -- self-reported -- how many breeches did they lose again (in which they bothered to report the outcomes?) Read that and then we'll talk about "OB emergencies" and the rate at which term neonates die in the USA.
One of the other problems, from my perspective, is that people seem to be conflating criticism of Dr. Amy's method of calculating/comparing figures with some sort of defense of MANA or home birth with inadequately trained midwives. See, for example, Trixie's comment. Where is Orac defending MANA or unqualified midwives? Yes, a lot of home birth advocates are also likely anti-vaccine, but as important an issue as that is, it doesn't play into the whole Dr. Amy/Jamie Bernstein conflict. So, please, folks, let's try not to conflate the two.
Perhaps Dr. Tuteur and her minions who've decided to visit for this post, given that several of them have clearly never read this blog or are not regulars, should know my opinion with respect to nurse practitioners, which, of course, includes CNMs.
http://scienceblogs.com/insolence/2014/01/14/on-advanced-practice-nurse…
As a pediatric resident, I remember caring for several pretty sick newborns rushed to the NICU from home births that were nowhere close to the hospital--and that distance (and transport time) almost certainly hurt those infants. The experience helped me realize that, if your baby suffers hypoxia during birth or goes septic shortly after, being in a hospital with a good NICU just down the hall is the best place to be. Period.
Oh, and as an aside about the use of the word "kerfuffle", this comment thread is the first time I've heard of it being a gendered and insensitive word. I've heard it used frequently to describe disagreements of opinion, regardless of the genders of the parties involved. Can someone who feels that it is a disrespectful or insensitive term please explain why? It's not a word I use often, but I'd like to be aware of the objections to it so I can take them into account if I ever do use it.
Orac, why should these "minions" read about your opinions on NPs? MANA doesn't encompass CNMs. The data deals with non-nurse midwives. Tuteur doesn't have a problem with CNMs -- maybe if you read her blog, you'd know that.
I've lurked on and off here for a few years and have commented infrequently. I also read over at Amy's site and comment there sometimes. I'm really disappointed in your response here. Not that you care, since anyone questioning your white knighting of Jamie Bernstein and who isn't part of the commentariat is clearly one of Amy's "minions."
I'm confused why nurse practitioners or CNMs have any relevance to the discussion of MANA stats. The whole problem is that MANA is an organization of (with a very few exceptions) lay midwives who are not CNMs. Hence the extremely poor outcomes (CNM home birth death rates are still higher than hospital rates, but much better than MANA's).
FWIW, I'm a regular reader here, although not a regular commenter.
Not at all. I've received some criticism from regular readers, too. However, I know a bunch of Amy's minions have arrived because (1) there are a lot of commenters today whom I've never seen before, virtually all of whom are criticizing me and/or defending Amy, and (2) I have my blog set so that the first time anyone posts the post automatically goes to moderation and I have to approve it before the person can comment without going to moderation first (for those of you newbie commenters here who wondered why your first post went to moderation). #2 has greatly cut down on comment spam, which is why I do it.
There have been a lot of first posts today that I've had to approve, more, I think, than I've ever had to deal with in a single day. So, I have data to back up my referring to "Amy's minions" coming over here. I could go back and count the number of notifications of such posts and provide an exact number if I were so inclined.
One strength (although some see it as a flaw perhaps) of Respectful Insolence is that Orac’s lengthy posts allow plenty of space to provide a great deal of background on every issue. I can come here for the very first time and read a post and really get the full picture of a subject. It’s never just “Here’s a refutation of a Burzynski testimonial” it’s more like “Let’s review Burzynski briefly and here’s a take down of the testimonial and this isn’t an isolated case, here’s a bunch of links to other similar breakdowns I’ve done.”
I would say Dr. Amy’s biggest flaw isn’t that she’s “nasty” as you say, but that she doesn’t fill in as much of the background detail with each of her posts. Her regular readers (and I’m one) know why she would compare high-risk midwife births to general hospital birth even if she doesn’t remind us of the fact in every post (it’s because the general culture of American CPMs is to either be ignorant of high risk situations because they don’t screen for them or to play off even twins and breech as just a “variation of normal.”). But it can be said that not every CPM practices that way, so perhaps it’s a stretch for Dr. Amy to make the comparison that she does.
Anyway, I can see why Jamie and her supporters want to portray this as “I said that the death rate was 4x and Amy says it’s 5.5x and now she’s being nasty and sending out the hounds.” Because if you haven’t been a regular reader of Dr. Amy’s, you would likely think Jamie’s in the right here.
But it’s about more than just the difference in relative risk figures. Jamie called out Dr. Amy on her credibility by saying her post was “sloppy and unscientific.” Dr. Amy’s work is not sloppy and unscientific. But because she doesn’t carefully lay out the background of an issue each and every time, and because Jamie Bernstein wasn’t the least bit rigorous in her own research before calling someone else out, we now have our own internecine skeptic war going on. Great.
To future skeptical bloggers who want to tackle this issue I’d say please do! Homebirth with underqualified midwives (ie CPMs, not CNMs who are indeed highly trained) is killing and permanently injuring more babies than vaccine refusal currently is, so the subject deserves a broad audience. But why make it about Dr. Amy? And if you want to make it about her, either read a lot of her old posts for background or ask her an email about whatever it is you don’t understand. Because she’ll definitely take the time to walk you through how she came to her conclusions.
So you have new commenters, people who read Amy's blog, none of whom are being disrespectful toward you or anyone else here, and you feel the need to derisively refer to them as "minions" ?
Which is not a valid reason to make such a comparison, as I have argued. All the "explanations" justifying it are unconvincing and come across as excuses for sloppy reasoning.
A "stretch" is putting it kindly.
Sigh. Disappointed. I'm a long time daily reader of both RI and SOB, and this is sad.
I'll say I'm more disappointed in Orac, though. Homebirth is not something he usually writes about, (in fact, I don't recall him EVER writing about it before) so this piece comes off as just a nasty little personal attack, especially when viewed through the lens of the past SBM issues.
I refer to my own commenters as "minions" sometimes, particularly pharma shills and minions. So does a longstanding commenter who created the joke. It's a longstanding in-joke. It's tongue in cheek. You guys are really easily offended, aren't you? That's odd, given how rough-and-tumble Amy's blog is.
From my experience, Dr. Amy is okay with Certified Nurse Midwives (CNM). She will usually point out the difference between a CNMs, which she sees as legit since they require a robust education, and Certified Professional Midwife (CPM) which are not require much beyond a High School diploma. Dr. Amy despises home birth in general and does not have much love for anyone that advocates it, be they CNM or OB/GYN.
I swear, I'm not a minion! I just have more input than usual today, since I happen to follow both blogs daily. Of course, that could make me an Orac minion, too. Can I apply for dual minionship? :)
MaryW:
Perhaps she's changed it since departing Science-Based Medicine, but Dr Gorski (the managing editor at SBM) is quoted by Orac in the OP as noting that Dr Tuteur had advocated for a more heavily moderated comment policy, and in fact he cited her own blog article on leaving SBM:
There is no "Comments Policy" page at Dr Tuteur's blog that I am aware of (usually such things are easily found, for obvious reasons), and since this is your claim to defend and not mine, I am loath to go digging through 3-4 years of posts to see if she ever posted something on the matter (either in a post or comment). Therefore, unless Dr Tuteur has changed her personal position on moderating in the interim, your statement appears to be incorrect. Perhaps you can link to a
post or comment where she has clarified changes to her moderation?
----------
With respect to objections to the use of the word "kerfuffle" (I am mostly considering T's comments, but not hers alone): apart from what anyone else has said on the matter, such objections are stretching mightily by characterizing Orac's criticisms of Mike Adams, say, as constituting a "debate" or "argument". Has Mike Adams ever followed up with a post of Orac's with a rebuttal using proper evidence and logic? Has Mike Adams ever had a principled debate with anyone (who has criticized him from the standpoint of science-based medicine)? I rather doubt it. (Although I would be pleasantly surprised to be wrong.)
----------
With respect to Irène Delse's specific comment "All that before Jamie decided to comment on Dr. Amy’s analysis of the MANA survey, not on the survey itself. It’s… interesting." and more general comments along that vein - bloggers will write about what they want to write about. Deal with it.
I recall reading a handful of commenters complaining about Ed Brayton (a former Scienceblogs blogger from before the National Geographic era) writing about Christians in the US attempting to override the Constitution, and going on wondering why he wasn't writing more about other religions behaving badly (where other religions was, almost invariably, one other religion - Islam). It was tedious and annoying blog-policing then (especially when, as with Irène's post, there was insinuation of apologia for unsavouriness). It's tedious and annoying blog-policing now.
Personally, I view global warming to be the single most pressing issue facing humanity today. You don't see me going around complaining that Dr Tuteur or others don't take global warming seriously enough, or complaining that their efforts to expose the seedy underbelly of woo-friendly midwifery in the US are a waste - because other people have different priorities in life than I do, and that's not just how it is, that's one of the things that makes life interesting and worthwhile.
----------
I think plenty of the criticism of Jamie Bernstein's post at GroundedParent is on point. But rebuttals to Bernstein on the basis of Skepchick's comments policy are pretty much a textbook case of a red herring - and, as I said upthread, you're on shaky ground indeed if your demarcation line for "who is a good/proper skeptic" is a blog comment policy.
----------
As a final word, kudos to everyone to took jane's claims (e.g. regarding Caesarean sections) to the cutting board and diced them up.
So you're expecting people who don't read here regularly and may be posting for the first time to understand why the author of this blog is referring to them as "minions." Got it.
I'm not easily offended, Orac, it's actually why I like Amy's blog, she tells it like it is. I work in MNCH in the developing world, it's why I like your output on vaccines. But you're wrong here on Bernstein, who can't math and couldn't even be bothered, by her own admission, to click on Tuteur's links.
Crud - I posted my comment #143 before I read Orac's at #141. Looks like dual minionship is allowed - huzzah! :)
It's not my fault if you don't know the culture, and I have neither the time nor the inclination to explain it to you, any more than, I daresay, Amy would have the time or inclination to explain it to me if I were to show up in her comments. Nor would I expect her, or any other blogger, to.
Also – I really dislike Dr Amy. She doesn’t know or understand anything about CNMs, except that they are all bad, only OB/Gyns should care for pregnant women.
Do you have a cite for that? I ask b/c every time I've seen Dr. Amy mention CNMs she's been positive towards them, and that she used to work with them when she was practicing.
I still want to now how someone like yourself would evaluate the conclusions from MANA in their study and whether it matched the data or not.
It seems to me that everyone is getting the same numbers for all practicable purposes so I really don't understand the disagreement from either Bernstein or yourself.
Orac, this is how I saw your bias/inconsistent snark/tarnishing your reputation as a skeptic…
(1) “This clearly confused Jamie at the time because she couldn’t find the equivalent numbers in the paper.”
When has “confusion” EVER been an excuse, especially when the person is supposed to be capable of doing an analysis? I mean, come on, the deaths are broken up by category in the MANA paper; the rate Citizens for Midwifery and Tuteur listed were totals. It doesn’t take a “stats junkie/guru” to figure out that you’re probably going to be adding them together! At the very least, a thorough person goes to the source. If Bernstein wasn’t capable/willing to do that, then she had no business writing this article. You would never excuse or softball this oversight if it were from, say, SaneVax. Yet that is exactly what you do for Bernstein.
(2) “I can find no flaw in this reasoning, and, had I noticed this first, I would have been far more snarky about it…”
As someone pointed out, there was a lot to find flaw with Bernstein’s analysis. She doesn’t use the same numbers as Tutuer and then ridicules her when her math doesn’t match. She clearly used 2.06, not 2.1; she clearly used .38, not .4. So how is it fair to call it a math error when 5.42 is the number Tuteur obtained (and we can guess is using Microsoft font size rules of numbers ending in .0 or .5) But I guess “Oh, Tuteur didn’t accurately round!” isn’t as zingy as “I seriously have no idea how Dr. Tuteur came up with 5.5x…”?
Further, Bernsteins “obvious reasons” for exclusion are not so obvious. I personally know that many hospitals do allow CNMs to take on VBAC candidates (UPMC, UCLA, AAMC). But, yes, there is the possibility of neonatal deaths of VBAC/breech/twins increasing the hospital rate. However, it would not be by much (consider that term breech trials in hospitals have nary a neonatal mortality.) Yes, it would be more accurate for Tuteur to characterize this as a comparison between hospital midwives and homebirth midwives. Yes, this doesn’t meet the benchmark of controlled science… but does that mean that we have to abdicate our ability to think and pretend a reasonable inference is ridiculous (as anyone who reads “OMGZ YOU GUYS” or “it’s not clear that we can get enough accuracy to the 1.6 per 1000 number to even determine that it’s truly ‘bigger’” would infer) just because there isn’t the “right kind” of science to back it up? Who are we now, Sherri Tenpenny?
(3) You completely ignore the fact that one of the reasons Tuteur called the piece a hatchet job was because in the original piece “Bernstein is off by more than 100 fold. 0.4 deaths/1000 is 0.04%. She added two extra zeros. The homebirth death rate was 2.1/1000, which is 0.21%. So the difference is 0.17%. That sounds like a tiny number, but when you are talking about thousands of births, it’s the difference between 4 deaths for every 10,000 babies born in the hospital and 21 deaths for every 10,000 babies born at home.”
(4) As a vaccine proponent, I don’t know how you could ignore Bernstein looking at absolute risk when the lives of children are at stake, with her saying, “This is a difference of 0.12 percentage point. [corrected absolute risk comparison] In other words, we are comparing an extremely small risk to a slightly higher extremely small risk.”
(5) You represent Bernstein's conclusion. "For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low" is NOT congruous to "The MANA data is legitimately concerning."
(6) "The Wonder database doesn’t allow one to look up the six week mortality, which is what the MANA paper reported.”
Bernstein made up the “6 weeks,” I’m assuming sloppily assuming the weeks from the breastfeeding part were the same as the deaths. The MANA paper clearly stated that it reported up through late neonatal mortality. By definition, that is 4 weeks and under (27 days) just like the CDC database. A basic, simple OBVIOUS error of Bernstein’s that you “trusted” was correct.
“Trust” is all well and good in its place… but its place is not with a self-identified skeptic on his self-identified skeptical blog where he is supposed to be, independent of style and snark, scrutinizing science.
Orac- a lot of us are here not to defend amy so much as to point out the problems with home birth, and specifically the MANA survey. That information is getting lost in these weird squabbles about what this person or that had to say about it and if that reflects poorly on them.
There are so many people here pointing out legit issues in this Jamie/Dr. Amy / Prof Orosz war. But the issues are again, being ignored.
I did not realize (until someone pointed out here) that Dr. Amy wrote on her blog about Grounded Parents and the Chris Breechen home birth stuff..... I wondered why Jamie had such an issue with Dr Amy b/c she made it SO obvious. As someone else pointed out, she was quite kind to MANA and saved all the snark for Dr. Amy in her post. And now it is all making sense. Grounded Parents *did* have a bone to pick with Dr. Amy and enlisted Jamie to fight back.
However, Jamie's analysis WAS sloppy. It is quite nice of you to try to save Jamie with your post here but anyone who clicks to read the blog posts will see the truth and see Jamie's lazy attempt to critique Dr. Amy's post.
You say this, Orac: "There’s just one problem, which has been pointed out by Dr. Amy, Jamie Bernstein, and Steve Novella. That problem is that, if you compare the death rates in the MANA study to publicly available death rates from other sources, the death rates in the MANA cohort are higher—and not just by a little."
But that is not true. Yes, Dr Amy and Steve Novella did point that out, that the home birth death rates are higher and "not just by a little." But that is not at all what Jamie said. Her conclusion was that home birth risk compared to hospital is "negligible or slightly higher." It's why MANA tweeted Jamie's post, for goodness sake!
And again, as I stated above, it is absolutely reasonable to compare hospital CNM births to home births that include women of all risk.
1. CNMs in hospitals can and do see high risk clients
2. It is a gamble for a woman choosing a midwife here in our country. It is not a matter of knowingly having a high risk home birth. It is an issue of women who do not know they are high risk b/c their midwife has failed them.
By you saying "All the “explanations” justifying it are unconvincing and come across as excuses for sloppy reasoning" it is really a slap in the face to the (too) many loss moms out there who unknowingly had high risk home births. For those of us (most especially Dr. Amy, who has been at this the longest) who see the devastation from home births and the families left just completely shocked and confused and utterly heartbroken, it's just.... it's what it IS. It is home birth in our country. It's a gamble. It's having no clue, really, what kind of midwife you get, what her track record is, whether she is giving informed consent, etc. As I mentioned above, I just had a new horrible home birth midwife story emailed to me about a midwife who straight up lied about two different test results that showed this woman was high risk. Withheld the information in order to not transfer her care.
Do you see this? Do you understand? Do you still think it's just "sloppy reasoning?"
The further irony being that the apparently objectionable engagement itself is cited by Dr. Tuteur as the very reason her presence was supposed have been perceived as some sort of existential threat to SBM.
LauraN - yes yes yes yes yes yes yes THANK YOU
"I'd object to it, but I've never heard it said."
Re: comment policy.
No, you didn't know there is virtually no moderation? That was my entire point, Narad. Hence the questioning of why Orac would talk about moderation policies, but not what was actually going on.
In all the years I have been reading SOB she has banned exactly one person that I am aware of, despite numerous insanely obnoxious trolls that everyone wished would just die in a fire already. Any longtime regular commenter can verify this. No matter how annoying a parachuting troll is, their comments stand. I have never seen her remove comment threads, and you can bet the regulars would shit bricks if she did because NOT censoring comments like ALL of the homebirth websites is a subject of pride among those that participate.
Composer99, the statement appears to be incorrect based on what you read here. Read her blog for a few years and get back to me on how many comments and users you see get blocked and deleted.
Perhaps Orac would care to explain what the real problem was with the 'moderation policy' at SBM rather than leaving folks to assume Dr Amy's goal was to censor the daylights out of anyone that disagreed with her.
Full disclosure, I found SBM via SOB when she started writing there, then found Orac via SBM. There was a very clear disparity in how her posts were handled vs. other contributors I could see from the very beginning, and applauded her leaving despite otherwise loving the site. I couldn't understand why her posts were handled so differently, though after her comments today there seems to be a little more clarity.
I am a first time commenter to this site, but long time reader. I've linked to both sites (SBM and here) more times than I can count, especially the articles on corn syrup and raw milk on SBM. I am a fan, especially as a fellow pro vax centered blogger, despite never commenting. If that makes me a minion and thus my critique less credible (which is what is implied by the usage) then fine.
I found this post so hard to swallow. Orac wants full disclosure from others, yet fails to do so himself. Giving such a huge pass to Bernstein is just ridiculous and goes against everything I've been arguing doctors DONT do for years. No, they don't collude with their buddies, they stick to the facts. End of story. Enter this post. Disappointing with a capital D.
I will continue reading, but it will be with a bad taste in my mouth, and a lingering question regarding veracity that this posed has raised.
Here’s the real problem with Berenstein’s piece. This “kerfuffle” with Dr. Amy (great word!) is a sideshow (and boring).
Berenstein spent a lot of time obsessing about how Dr. Orosz didn’t have exact groups that matched the MANA dataset in every way. But then she never admitted that the assumptions made by Dr. Orosz, which were clearly laid out and never hidden, were always in MANA's favor. Always.
So you can’t calculate an exact p-value. A good statistician half-disbelieves p-values anyway. I can still see that, even when Orosz assumes a value of 0.3/1000 for intrapartum stillbirth based on the WHO's estimate (which is supposedly too high), that the MANA data set (which is highly self-selected) gives a value of 1.3 (!) for supposedly low-risk women. And that is for something that is considered to be extremely rare in the world of modern obstetrics. I don't need an effing p-value to be shocked. I can still see that, for women that MANA is claiming are low risk, that the neonatal death rate is 0.77 and higher than that of low and high risk women delivering in hospitals, which is 0.41. (I don’t know the CI).
You know what I would call someone in a lab meeting who was obsessing about the inexactness of the comparison, but refused to admit that it worked in one party’s favor? Obtuse.
No one really believes that there is enough data on US homebirth. But what little data we have is suggestive of major problems on multiple levels, at least where CPMs are concerned.
I am not an epidemiologist. I work in a field (experimental genetics) where I can manipulate my subjects. I’d like to think that I am able to keep the handwaving to a blessed minimum. But I never allow a criticism of a method to pass in a lab meeting without demanding that the person making it explain exactly how it could bias the results one way or another, or indicate another serious problem, like lack of power. Anyone, even a self-described “statistics junkie” can do the former, but considering the implications requires deeper engagement. Berenstein did not rise to that level of analysis.
Love your blog, by the way! Keep up the good work.
Since it's been brought up several times, regarding Dr, Tuteur quitting SBM and the moderation policy...
Dr. Tuteur in 2010:
Dr. Tuteur now:
There's no excuse for it, and I'm not just saying that because it's a Gurl Thang.
If you can't engage in a debate about a difference of opinion and/or understanding with the peers and fellows in your community without going from zero to ad-hominem in the opening round, why are you even in a community dedicated to fact and reason to begin with?
There's a milieu for people with that kind of temperament already. It's called the House of Representatives.
Oh, sorry, I thought your point was what you said:
That's why I mentioned Dr. Tuteur's assertion that people are kept in line at her place, unlike the SBM rabble, because they know and fear the banhammer.
I will reiterate my final point: Why would you expect anyone here to be familiar with this? I probably became aware of Dr. Tuteur here some time ago or back when I was reading SBM (before the redesign), but it didn't cause me to add her blog to my regular reading, much less follow the comments so as to try to infer the underlying psychological boundaries of acceptable conduct there.
Yes Narad, I amended my statement because I was aware of a single person being banned. In years. But way to miss the point entirely. Again.
Do you actually see anyone contradicting them?
As a student nurse-midwife, I can tell you that CNMs absolutely attend VBAC and twin (although only di-di twins) births in the hospital.
Also births of gestational diabetics, obese women, women with pre-eclampsia (who do not have the severe features of the disease), women with hypertension, women with thyroid problems (usually only hypothyroid)...there are plenty of high risk women being cared for by CNMs. They often consult but continue to manage the patient and the delivery.
She's not exactly a stickler for keeping things fact-and-reason-based, is she?
It's not clear to me that you have a point in this regard when you're disgorging things like this:
I'm not aware of anyone here who really cares how she moderates her comments. It was her choice to leverage this "proximate cause" – i.e., SBM wasn't moderated to her liking and wouldn't give her the reins and so there were comments that never would have seen the light of day on her watch – into some weird screed about how she was cast out lest the Corona Borealis return from the heavens.
Mary W:
As I said, the claim "Everyone is aware that Dr Amy’s own blog is completely unmoderated, yes?" is yours to defend. It is not mine to disprove. In light of Dr Tuteur's own words to the contrary - "The sticking point was the lack of a moderation policy. [Emphasis mine.]" - the onus is on you to substantiate your own claim - that is, that The Skeptical OB comments are completely unmoderated, rather than lightly moderated (as explicitly described by Dr Tuteur).
At any rate, both Dr Gorski's comments at Science-Based Medicine and Dr Tuteur's comments on her own blog with respect to the moderation policy at SBM pretty much lay it all out.
Dr Gorski: "However, since Amy has cited our moderation policy as a reason for her departure, I no longer see a reason not to confirm that one unresolvable issue was that Amy strongly favored a more heavily moderated commenting system, and Steve and I were very reluctant to change our commenting policy."
Dr Tuteur: "The sticking point was the lack of a moderation policy. Every comment thread spun out of control because certain people (almost all of whom came from here) were free to post garbage that they could never get away with on this site."
So I really can't understand what more Orac ought to say. Both Drs Gorski & Tuteur agreed on what the problem with the moderation policy at SBM was - there wasn't one to speak of at the time. Given that, as Dr Tuteur noted, such moderation as she had undertaken to date was extremely light, and Dr Gorski quoted her in full writing that, I can't see how you can reasonably conclude that Orac highlighted that passage to impute sinister, censoring motives to Dr Tuteur.
As far as I can see it was to draw attention to the "it's a bit rich"-ness of Dr Tuteur having advocated for a stronger comments policy at SBM now calling out Skepchick for engaging in "censorship" on account of its comments policy.
Exactly. That's it. Nothing more.
WON'T SOMEONE THINK ABOUT THE CHILDREN!!??!!
I thought we were thinking about the children...
Isn't that the whole reason for this discussion? :-)
Oh my.
(Just read her response.)
I count zero sentences that don't include wholly extraneous personal drama about incidental crap, plus four with a token gesture in the direction of the topic towards the end.
That -- ie, the OP, above -- is not a screed, by any stretch of the imagination. I would have called it mild, in fact.
And it's all directed towards the substance of what she wrote, said and did, as reflected in the extant public record, ffs. It's either right. Or it's wrong. Fair. Or unfair.
How complicated is that?
Embarassing.
Still no (meaningful) responses from Orac. I keeeeep checking....
For really reals, me either.
It's obviously there to highlight the apparent double standard.
I mean, I wouldn't be happy if it were about me. But I don't go around crying censorship, unless freedom of speech is being imperiled.
False accusations of censorship. Now there's a pandemic.
Ah, but now that the abreaction has come, we know that there was one: Everybody except Dr. Tuteur was moderating SBM comments (emphasis added):
"They wouldn't let me moderate comments on my posts although they did moderate on theirs."
That's not an accurate paraphrase. And arguably not a fair one. She specified low-risk births when saying that, surrounded it with qualifications, and finished off by saying that there was evidence rates for high-risk births were "much higher" -- ie, higher by more than a little.
You know, if this were just an argument on the merits, it wouldn't be much of one. Possibly the skepchick piece is a little too fair to MANA.
If so, is there some reason why a collegial exchange of emails and elucidation among chums couldn't have led to some minor emendations and hat-tips all around?
There's barely any snark in the Jamie Bernstein piece at all. I see (maybe) one example, plus one charge of sloppiness, which -- while quite possibly wrong -- clearly reads (at least to me) as an honest mistake, if it is one.
I always thought "kerfuffle" was a Yiddish word. But it turns out to be of Gaelic origin.
You learn something every day.
PS -- If any guy ever disrespects my authoritah by using that word in reference to any of my very serious undertakings, I'll menace him with a rolling pin. Don't say you weren't warned.
Ann - this is Jamie's exact conclusion "For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low. For high-risk births there is some evidence that neonatal mortality rates could be much higher in a homebirth setting compared to a hospital."
As I read it on her blog, there was an issue that SBM moderated comments but did not allow her posts to be moderated, which hasn't been addressed at all. That disparity in treatment was what she claims the actual problem with the moderation policy was, though that bone of contention wasn't really the main issue. By all means keep quoting her attempt at civility from 2010 instead of paying attention to what she says actually happened as of today.
The onus is on me to prove a negative..that people aren't censored or banned. .I'll get right on that. Or maybe go over to SOB and ask everyone there, including Dr Amy.
Is Amy lying about the moderation disparity? I don't know, but Orac hasn't confirmed or denied it. Seeing how he would pounce on her posts that he personally approved, coupled with the actions here, it doesn't make her case sound particularly unlikely.
We already know from the UK Birthplace study that, for first-timers, even with a tight risk-out policy and 40% transfer rate, the neonatal mortality was 3x greater. On what basis could a journalist claim that the MANA stats show this to be ''negligible''?
From a pediatric point of view, I don't get why, after 9 months of pregnancy, where--if you are at all in touch with science-based medicine you've been getting prenatal care all along--that you would then go and risk it all with an at-home birth. Bad stuff can happen during the delivery. You need someone trained and experienced in every possible complication that could occur during the delivery. And, after the delivery, wouldn't you want someone who knows how to resuscitate a newborn if needed? You don't get that by having your baby at home. You do get that by having your baby in a hospital.
They're quoted right next to each other. So it's not really an either/or. Besides. you know what I think is the best way to avoid having people quote you saying stuff that contradicts what you're now saying?
Don't say it.
Also, I think you're being a little unfair to her. It wasn't just an attempt. It was actually civil.
Don't trouble yourself. Because:
(a) Nobody is alleging that people are censored or banned; and
(b) Censorship involves the suppression of speech, which is a literal impossibility in the context of blog comments on the internet, where numerous other venues are available to those whose posts include content that moderators disallow.
If you like, you can take upon yourself the onus of defending the assertion that the blog is "completely unmoderated," though. I don't think it's, like, a pressing need or anything. Ad it's obviously not of much moment. But the suggestion was made.
It's considered good form to produce evidence that a bad act occurred before demanding confirmation or denial of it, when suddenly accusing people of misdeeds out of the blue years after the fact while in the midst of pitched personal conflict.
Otherwise, everybody might just go around pitching tantrums and saying whatever shit suited their immediate needs whenever they felt like it.
It's called "editing." And I don't see how (coupled with his actions here -- which are called "writing") it has any bearing on the question. So I'm not sure where you're getting that. Is there a quote you could point me to?
On no conceivable basis, since the MANA stats are from a different study of a different sample in a different country, conducted, designed and written by different researchers.
I imagine that's why no journalist has claimed it.
Chris, many people who homebirth are told over and over again that birth is as safe as life gets, that 'physiological birth' is safer than 'medicalized birth' because your baby is gonna get all drugged up by your drug pushing shifty eyed anesthesiologist http://www.midwiferytoday.com/articles/epiduraltrip.asp) . That it's just as safe to deliver at home than at a hospital and anyone saying otherwise is threatened by midwives or is one of the overmedicalized sheeple who don't trust birth or their body. That babies know when to be born, that your body won't produce a baby too big for you to birth, that the only real complications of birth happen because of the 'cascade of interventions', because they're not in a comfortable environment, because they're being observed (according to these folks people are animals who can't safely give birth if they know they're being observed), that if you're in the hospital you will be strapped down and surrounded by tubes, forced to labor on your back, hungry, thirsty and miserable while your ob just treats you like a paycheck and wants to get to his tee time.
Oh and cause they watched The Business of Being Born, which repeats a lot of the above tropes as well.
Ann, are you familiar with the coverage of this issue? Because most of what I've seen has simply gone along with MANAs assertion that homebirth has fewer interventions and is safe. Since your pedantic, that's not a direct quote. But here are some articles
http://www.mana.org/blog/home-birth-safety-outcomes
http://m.huffpost.com/us/entry/4696665
(Which changed the title after it was pointed out how misleading it is, and the study actually didn't find 'no increased risk to ...baby')
http://www.examiner.com/article/new-and-largest-study-finds-home-birth-…
(This one is accurate as there's not an increased risk to women, though there's also not a decreased risk as someone upthread sugvested, either. No mention is made of risk to baby)
Also, when called on having compared a cohort of low-risk hospital births to a cohort of high- *and* low-risk home births that she represented as a like-kind to like-kind comparison, Dr. Amy replied:
Yeah. Here's another crazy idea. If you want to unilaterally redefine what are commonly understood to be the objective real facts of the subject you're discussing in order to make your point, make a note of it so that readers know that's what you're doing.
That way they won't have to ask. And you won't appear to be making misrepresentations.
Plus, producing your unsourced personal justifications after the fact usually doesn't cut it in science, per my understanding of the thing.
It seems that everyone agrees that home birth carries much higher risks than hospital birth (except, perhaps, for Ms Bernstein) and yet we are still arguing. A good deal of that centres on the style of Orac and Dr Tuteur, and yet both tend to trample on the sensitivities of those they criticise in the name of truth and clarity. The one thing I find strange is that Skepchicks/Grounded Parents should have chosen to take on Dr Tuteur - they are supposed to be on the same side. But when you consider that Dr Tuteur is an old school successful professional woman who built herself a successful career without crying out that she was being oppressed all the time, and that the self-proclaimed Skepchicks are rather light on life experience, real jobs, and actual involvement with science, it becomes understandable. Hipsters who think sciencey stuff is cool, but find actual thinking hard, would presumably feel threatened by a tough old broad like Amy. At the end of it all, the point for them was click bait, and Grounded Parents has achieved its aims in that regard. I find it reprehensible that they would take a pro-woo position by minimising the risks of homebirth for such a reason.
Ann what kind of source do you want for what homebirth midwives are actually counseling patients? Do the patients own stories count? If members of an organization is acting counter to how they claim to act and doing so dangerously, why SHOULD we give them the benefit of the doubt? It's not as if they're going to give you a 'study' showing their negligent behavior.
*are acting
This is the conference program for an upcoming Midwifery Today conference, where CPM midwives receive continuing "education." If you peruse the topics you'll get a good feel for what CPMs consider to be well within the scope of their practice. http://www.midwiferytoday.com/conferences/Harrisburg2014/program.asp
Diane Goslin, a CPM midwife who practices alegally in PA, is teaching workshops on how to do breech, VBAC, and twin births at home. Here's the grand jury report detailing a few of the deaths and severe injuries Diane Goslin caused to babies over the last several years. http://www.scribd.com/doc/176703928/Lancaster-County-Grand-Jury-Report-…
You'll read how she coached several immigrants with a poor command of English, and Amish patients without a great deal of science education, to trust her judgement in not administering antibiotics for Group B Strep infection, for example. This is the BEST that MANA has to offer. They make her a teacher and invite her to share her wisdom with others.
This is why Dr. Amy feels it's appropriate to include high risk deliveries in the comparison. Because home birth midwives don't consider breech, VBAC, and twins to be high risk. They happily forge ahead with delivering them at home.
Trixie @189 -- it's awful stuff like this that makes my wife wonder if it might have been wiser to call Certified Nurse Midwives something else, which doesn't have the word "midwife" in it.
Lancelot Gobbo @186 -- Yow.
I'd want whatever the source happened to be. "According to what more than a dozen patients have told this writer," would be fine. And "according to a former longtime member and ex-midwife" would be fine. And "according to an investigative report published in the Daily Blat-Spokesman of East Someplace, USA" would also be fine.
The point of sourcing is to give the folks some indication of how reliable the information is and some means of checking it themselves.
Who said anything about that? I thought we were talking about sourcing the claim.
No. But there are these two options:
(1) You have knowledge of their negligent behavior. If so, it necessarily comes from somewhere known to you, which you can state while relaying it to others.
(2) You don't have knowledge of their negligent behavior, in which case it is itself negligent behavior to suggest that you do.
Unless it's just your surmise, which you state as such while making the best case for it you can, on reasonable grounds.
Or whatever. There are lots of ways to go, really. It's just the unsourced allegations that are problematic.
Ann, I have blogged extensively about midwives in utah discouraging vaccination (which is in direct opposition to the state health departments vaccination campaign), as well as crowd sourcing conditions that are well outside their scope of practice (like pelvic organ prolapse during pregnancy, hernias, liver conditions, etc).
Heres my piece on the anti-vaccination bent of the midwives organization and the president of the midwives college of utah (who is also on the MEAC board if I recall correctly)
http://safermidwiferyutah.wordpress.com/2014/02/03/60/
my two previous pieces are about the idiocy these women display openly on the internet for all to see.
When they were asking for CPMs to legally deliver babies in the state they straight up lied and said they did not practice medicine and would never go outside a reasonable scope of practice, but they do, all the time. I personally got told not to get a flu shot by a CPM while I was pregnant.
On yeah and Ann- follow ANY major CPM group on facebook. Crowdsourcing decisions on facebook that are far outside the scope of practice is absolutely the norm for CPMs. It isn't professional or ethical, but it what they do. One of the worst ones I can remember (outside of the recent death that occurred because of 42+ weeks and no amniotic fluid) is a woman with a bleeding disorder and a metal bar in her sacrum from a previous surgery. They were all brainstorming ideas for this woman to have a home birth despite the obvious worry of PPH involved with a mom on blood thinners.
If you don't think negligence is the norm, you just haven't look around much.
The worst part is a lot of them don't even say "consult a doctor". They say "use stevia" or "lemon juice" or "pilates" or "homeopathy". Worthless ideas that could kill someone.
Hey!
Citation of over-precision on my part, or quit it with the unprovoked ad hominem, please.
I'll be happy to concede the point if there is one.
Thanks. I'm inclined to the hospital-birth side of the debate already.
"On no conceivable basis, since the MANA stats are from a different study of a different sample in a different country, conducted, designed and written by different researchers.
I imagine that’s why no journalist has claimed it."
Ugh but don't you see? These were numbers from midwives with LESS training, NO risk out policy, who only filled out the survey on a voluntary basis and without any peer review. It is absolutely reasonable to think that the actual numbers are higher in light of that, and in light of poor outcomes being demonstrated across the board in systems with better trained midwives who are actually integrated into the health care system. Every advantage available to improve the safety of out of hospital birth is absent in the US when using a CPM. I don't know how you could choose to be purposely obtuse about the meaning of that.
oh, and for the record, Dr Amy calls CNMs "real midwives" because they adequate training to do what they do. People who think she hates CNMs have not read her work- its a major point of her writing is to clarify the difference between Nurse Midwives and CPMs.
Trixie @189: I have always considered the Amish a bit of an anomoly among homebirthers. I live in an area filled with the Amish and have fairly ongoing contacts with them for some matters.
Depending upon the order, the Amish range from accepting of medical care when needed all the way to never accepting it. I have come in contact with a midwife who performs homebirths for the Amish (including those in the high-risk groups). Her theory for assisting them largely falls into the catageory of Harm Reduction. She pointed out that many of these people, especially those in the Old Orders, would not go to a hospital under any circumstances. If no midwife could be located to assist with the birth, they will rely upon other community members or proceed unassisted. A complicating issue here is that the Amish as a group rarely, if ever, carry insurance so going to a medical professional can likely destroy their financial security.
The midwife I met stressed to me repeatedly that she does not attending these births and wishes the people would go to the hospital. However, she emphasized that she feels like there is an ethical duty to at least try to mitigate the harm that could occur. Refusing to see the patient would largely just result in unassisted birthing, a far more dangerous situation. She compares it somewhat to the idea of harm reduction in other areas, which basically acknowledges that some people will not be turned from pursuing a bad or dangerous practice and in those cases, it may be more ethical to engage them on their own terms and attempt to minimize danger within the practice.
I am not sure I particularly agreed with her on all grounds, but I did find the argument interesting.
@safer midwifery utah --
(and anybody else who's considering going the same route)
I haven't said jack about any of those issues, or -- in fact -- about midwifery. There's no reason to assume I dispute them, therefore.
Where the f'ing f did I say, suggest or hint I didn't think negligence was the norm?
What I object to is people throwing unsourced allegations of wrong-doing at their ideological foes and/or personal enemies.
Because that's a witch-hunt tactic, among other things.
.
Although the unsourced thing is minor relative to changing the terms on which the cohorts are being compared all on your ownsie without saying so.
Because people can always ask for a source, if they need one. And it might be a legitimate oversight. Or editorial choice, if it's safe to assume an informed readership.
But there's no such thing as legitimately authorizing yourself to use words from your own private language, the true meaning of which is known only to you.
It's misrepresentation.
OneOther, it is true that Amish will home birth by default except in the case of severe risk factors. However, in the Goslin case, it's worth noting that in Lancaster County there are many CNM midwives with hospital privileges, an accredited birth center, and backup OBs who operate within the law and have excellent outcomes. They attend home births for Plain sects as well as the "English." In the grand jury report above, Rita Rhoads, the CNM who testified against Goslin, is a Mennonite CNM who opened Birth Care over 30 years ago, precisely to fulfill a need in the Lancaster County Amish community for safe(-r) home birth. Birth Care's board of directors is made up of many elders in the Amish community, as well as medical professionals. They risk out patients appropriately, push vaccination, and admit patients to a local hospital that is Amish-friendly when necessary. So while I understand what you're saying about risk minimization in the Amish, the truth is that in Lancaster County, where Goslin operates, there is generally a very good relationship between the medical community and the Amish, at least among a subset of trusted providers such as Birth Care and the Clinic For Special Children run by Dr. Holmes Morton. This may not be the case to the same degree among more isolated colonies in other parts of the country.
Ann, is pedantic an ad hom? I rather consider it a compliment. I do find your participation in this thread somewhat frustrating, but it's not your fault that you are less familiar (and thus less burned out at rehashing the same points over and over) with this debate, and I Don't fault you for wanting sources. Are what's been provided since I posted sufficient or would you like more examples? One good place to look at is http://hurtbyhomebirth.blogspot.com/?m=1
Anyone who doesn't understand that woo is INHERENT in the CPM credential (as apparently Orac and his apologists do, especially when they pompously conflate it with a CNM credential) is very ignorant on the topic. Consider this "course schedule" from a midwifery school:
"21. Pharmacology I: American Herbal Pharmacology (12 hrs didactic, 12 hrs practicum)
22. Pharmacology II: Homeopathy for Midwives (12 hrs didactic, 12 hrs practicum)...
23. Pharmacology III: Intro. to Traditional Chinese Medicine (18 hrs didactic, 6 hrs practicum)...
24. Pharmacology IV: Intro. to Allopathic Pharmacology (18 hrs. didactic, 6 hrs practicum)"
What science-valuing person would be comfortable conflating the equivalent of a nurse practitioner with someone who has more training in woo than actual pharmacology? One more concerned with knee-jerk defense of his/her "champion" than a thorough understanding of the issue; more concerned about digging in or deflecting than admitting error.
Tuteur may have qualms with the American College of Nurse Midwives for obfuscating studies that are unfavorable for the OOH members, but she has always referred to them as "real midwives" and real health professionals. Really, these comments make it more and more obvious that Orac &Co. will jump on anything they think will vilify Tuteur and deflect from Bernstein's overall ineptitude and obfuscate the conclusions she presented: "For low-risk births the neonatal mortality rate of having a homebirth is either NEGLIGIBLE or SLIGHTLY [emphasis mine] higher than that of a hospital birth..."
I'll be sure to be comforted when an unvaccinated child dies of influenza because the mortality rate of influenza in unvaccinated is only "slightly higher" than in the vaccinated. Oh, wait, all of a sudden we want to look at relative risk and consider risk vs. benefit in our analysis? Well... that's consistent...
If so, she should say so, while *also saying that's what she's doing.*
Because if I were reading a critique that justified such a comparison on those grounds, the questions that would occur to me would be: "Do patients with a poor command of English and/or very little science education get significantly better treatment from mainstream medicine in practice? Or just in theory?"
And that wouldn't be because I was pro- or anti- anything besides all patients getting good, responsible medical care.
Which I'm for.
I meant "medicine," not "mainstream medicine."
I just started to attempt wordplay and forgot to delete it.
I don't see anybody doing that at all, let alone anybody doing it pompously.
It's more than possible I missed it. But it's not even distantly possible that I missed "Orac and his apologists" doing it.
It would be nice to be engaged on the arguments actually being made, if it's not too pedantic to ask.
Um, Ann, she did: "We cannot remove breech, twins, VBAC, and other high risk conditions from the homebirth group because homebirth midwives are publicly on record claiming that these conditions are “variations of normal” and have lobbied across the country to have them included in homebirth midwives scope of practice."
http://www.skepticalob.com/2014/01/the-many-deceptions-large-and-small-…
And, yes, that was published before Bernstein's inept article and Orac's uncritical knee-jerk defense of her inept article.
Ann, see post #131:
"Orac
March 13, 2014
Also – I really dislike Dr Amy. She doesn’t know or understand anything about CNMs, except that they are all bad, only OB/Gyns should care for pregnant women. I had several run-ins with her years ago, when she blatantly mis-represented what CNMs are taught, and she both refused to recant or apologize. So I won’t read her writing any more.
Perhaps Dr. Tuteur and her minions who’ve decided to visit for this post, given that several of them have clearly never read this blog or are not regulars, should know my opinion with respect to nurse practitioners, which, of course, includes CNMs.
http://scienceblogs.com/insolence/2014/01/14/on-advanced-practice-nurse…"
Trixie, I think the article doesn't make a lot clear. There are various Amish sects, and one thing that surprises many is that they do not all get along. In fact, among those who study them, it's actually functionally incorrect to say "The Amish" since they are so diverse.
Lancaster's medical system has a very good working relationship with the Mennonites (who it must be emphasized are NOT Amish) and the more open Amish sects. The largest issues come from the most traditional Old Order sects that eschew all forms of medicine. Most liberal or open-minded Amish could certainly be convinced to go to a hospital in the event of serious need. However, there are those who will not. It's not a matter of whether the medical community has a good relationship with some of the sects present in Lancaster. The issue is that there are groups that would refuse to go under any circumstance at all.
Is Orac commenting as Ann in disguise in attempt to totally derail the conversation with pure nonsense, just to avoid answering some of the clear issues with Bernstein's posts?
Orac agrees with Dr. Tuteur and Steve Novella: home birth is too risky.
That is squashed. They agree. Awesome.
What hasn't been addressed - AT ALL - are the many issues with Bernstein's posts, which have been pointed out in the comments by MANY both at Grounded Parents and again here. And again, the issues/concerns/errors regarding this are being ignored.
Orac, we are all still waiting for you to reply to some of the very good, very valid comments regarding the "kerfluffle." Like the following comments:
#17 by EBA
#50 by EBA
#150 by LauraN
Also, just to point out again to Ann and Orac and anyone else - Bernstein's first post IS far too kind to MANA and very harsh to Dr. Amy, her conclusion ("For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low") did NOT agree with Steve Novella, Dr Amy and Orac
and THIS IS WHY MANA TWEETED JAMIE'S POST: It makes Dr. Amy look bad, MANA look good, and home birth look safe.
Orac, you are screwed now. There are no minions more vicious or more loyal then Dr. Amy minions. All she has to do is a post a link and hundreds come flocking, ready to battle for days and weeks on end to defend her.
Birth is a very emotional topic for women. That's a fact. Everything is taken personally; everything is an attack on them as mothers. But I digress..
First of all, the neonatal mortality rate for low risk women at homebirth (according to many) is 0.7/1000. Compare that to the neonatal mortality rate of low risk women at the hospital, and we ARE talking a small difference. 0.7 compared to around 0.4/0.5. The intrapartum mortality rate for low risk homebirth is 0.8/1000 and for low risk hospital birth it is 0.3/1000. That is more significant. But it's something that Dr. Amy leaves out of her blog posts and she knows it too. So you really aren't comparing 0.4/1000 to 1.6/1000. You are comparing 0.7/1000 to 1.57/1000. Homebirth does not have 5x higher mortality rate or a 4x higher mortality rate. It has a 2x higher mortality rate. I think you should edit that in your post. Those are the real numbers and it just goes to show how dishonest Dr. Amy really is.
*and I know her minions will freak out about this but it was doctor Orosz who stated the intrapartum mortality rate for hospital birth is 0.3/1000. Dr Amy tried to claim it was zero! That's impossible. That would mean that no babies die in labor in US hospitals. And secondly, that number is purely an assumption on Dr. Amy's part.
*accrding to MANA
rancidbrainmatter I’ve had three home births–results now aged 40, 36, and 28. Come and get me Mu.
That's like bragging "I drove drunk with my kids in the car all the time, nothing ever happened".
OneOther, I'm pretty familiar with Lancaster County Amish culture and Anabaptist culture in general, and your assertion that Old Order Amish will not go to the hospital no matter what is incorrect. There may be individual variation in what medical treatments people accept, but those fall under individual preference rather than religious edict or official belief, just like Amish attitudes towards vaccination. The main reason they avoid hospitals is because they pay out of pocket for medical treatments, and home birth is cheaper for them. If you read the grand jury report, you'd also see that only 1 of the 3 cases in question involved Amish at all, and that Amish family did take their baby to the hospital for treatment when they realized the seriousness of the situation. Sylvia Stoltzfus, the mother, consented to GBS testing, and was open to treatment, but Diane Goslin never gave her the results that she tested positive and never treated her in labor (pages 13-14). The point is that Goslin is not a "better than nothing" provider and the Amish are not a special case.
But this isn't just about CPMs preying on the Amish. CPMs prey on educated upper middle class people the same way. Wren Jones died of Group B Strep after a CPM midwife advised the parents to treat it with garlic and not antibiotics. http://www.dreamhost.com/dreamscape/2011/03/09/wren-jones/
@LauraN, #208
I think you may be reading more into those comments than is actually there.
I don't read Dr. Tuteur's blog, so I can't say whether she actually denigrates CNMs or not, but if that's untrue as many have suggested (and I'm willing to give that the benefit of the doubt) then that simply means that the commenter who originally claimed she does that may have been mistaken or interpreted legitimate criticisms of CNMs as unduly harsh. Or is it possible that Dr. Tuteur's opinions have evolved over time and her older posts are more critical? Either way, there are a variety of reasons for why that commenter might have felt that way and it's hardly evidence of a coordinated conspiracy against Dr. Tuteur, especially since that's the only commenter I've seen make that claim.
As for Orac's comment, I'm a bit unsure as to his intent as I obviously can't read his mind, but I don't see how it supports your position that he is conflating CNMs and CPMs and doesn't recognize how much woo CPMs are trained in. That article is supportive of NPs and expanding their scope of practice precisely because they have proper science-based training. Based on that, and my experience as a longtime lurker here, I can't see him having anything but scorn for CPMs, even if he doesn't directly state it because obstetrics is simply something he doesn't talk about much (though I hope I'm not putting words in Orac's mouth :))
Though I'm open to being persuaded otherwise if you have some good evidence
Orac, why not ask Dr. Amos Grunebaum to weigh in? He's a well-respected OB with none of the blogger baggage that seems to be dragging this issue down between you and SOB right now, and he's publishing research on home birth death and injury rates. http://www.livescience.com/43050-home-births-newborn-death.html
Dr. Amy has a lot of respect for CNMs. She has *many* CNMs that are regular readers of her blog and are in the Facebook groups started by Dr. Amy. She has a guest post today by a CNM. She regularly refers to CNMs as highly trained and highly skilled and the best midwives in the world and that CPMs are an inferior midwife.
Here is an example, written by Dr. Amy about CNMs:
"If you are worried about the health and safety of your baby and yourself, you would hire a healthcare professional, like an obstetrician or certified nurse midwife (CNM), who has years of specialized education and training, and is governed by state regulation and professional ethics that place your well-being above their profit and their preferences."
http://www.skepticalob.com/2013/03/birth-workers.html
Trixie - I think you're misreading what I said. The Amish lifestyle is incredibly varied. The Ordung is not set in stone. The Ordung rules can vary from town to town and sect to sect. At no point in my comments did I say that the Amish as a group refuse medical care. What I pointed out was that some sects, particularly within the Old Orders, refuse all medical care. Your point about good medical care is moot in that context because such individuals would never avail themselves of care regardless of how good it is. Your initial comment expressed anger that midwives will attend to such people when they are in high-risk situations. I was pointing out that in such cases, at-home midwifery care might possibly be encouragable solely under a "harm reduction" theory that allows such people access to care in their chosen environment.
There's no Ordnung that requires any Amish group to refuse all medical care. That's just false. If you can prove otherwise, I'd love to see your evidence.
At any rate, it's irrelevant, because it wasn't the case here. Not only was the mother open to medical care, she consented to GBS screening and stated that she would have consented to antibiotic treatment if she had been informed. There's no sect of Amish in the area where Goslin practices who won't see a CNM out of some type of Ordnung. The real issue boils down to Goslin charging about $1,000 less per delivery than the CNMs do, because Goslin doesn't bother with pesky things like insurance or proper medical equipment and training.
Dani @ 217 - My impression of Dr. Amy and CNM has always been that she is amendable to them - as long as they practice in hospitals or hospital-attached birth centers and can be supervised by an OB. She is extremely against the small number of CNMs who perform homebirths and is also not a fan of those in freestanding birth centers. That leads many people I've encountered to argue that she tolerates them, but certainly views them as inferior to the OBs, who receive surgical training. I've never seen her mention on the blog that CNMs are equivalent to OBs in terms of training or skill. This sets up the argument that some people make that she merely supports the "illusory" midwife birth - let the little lady have her CNM in the hospital until she needs intervention and then the doctor will swoop in and help her.
I have always understood reading SOB that a CNM is preferrable to a CPM or DEM. However, I've never seen anything on the blog discussing the differences or equivalencies between CNMs and OBs, which is something I'd be deeply interested in seeing.
it was doctor Orosz who stated the intrapartum mortality rate for hospital birth is 0.3/1000.
Actually, if you read Prof Orosz's analysis in full, she said that it was very difficult to determine the intrapartum mortality rate for hospital birth and she was using a high end estimate. Prof Orosz's analysis was designed to give the best possible assumptions to home birth whenever there was uncertainty in order to avoid a false negative (attributing risk to home birth when there was none.) The rate of IP mortality may well be closer to zero, especially for low risk births, but it is certainly no higher than 0.3/1000.
As far as comparing low risk births to low risk births, I agree that it can be very difficult and that the MANA data is confusing and difficult to compare. However, if you go to CDCWonder, it is easy enough to compare "apples to apples" in a way that guarantees equality of risk.
The following is a search by medical attendant and birthplace for white women age 20-44 who are married and have at least a college degree (i.e. a demographically low risk maternal population, though, of course, this gives no info on comorbid conditions, etc.), with birth at at least 39 weeks GA, 2500+ grams birth weight, and at least some prenatal care.
The results show a neonatal (0-27 days) mortality of 0.40 for doctor/hospital versus 1.07 for other midwife (not CNM)/out of hospital. That's a bit more than 2.5x relative risk for home birth. Add in the intrapartum data, making the assumptions most favorable to home birth (i.e. IP mortality of 0.3/1000 in hospital) and you get 1.87 versus 0.70, for an odds ratio of about 2.67. So the relative risk can't be less than 2.67. But one should also consider that patients who see OBs may be higher risk (medical issues, prior problems with childbirth, etc). So a more fair comparison might be CNM/hospital versus other midwife/out of hospital. CNM/hospital has a neonatal mortality of 0.26, making the odds ratio for patients cared for by CNM in hospital to non-CNM out of hospital 4.12. It looks a little better if you add in the probably falsely elevated hospital IP death rate, but it's still a ratio of 3.3.
If you disagree with my analysis, tell me where you think I'm off. But if not, tell me, do you think that a relative risk of up to 4x is trivial?
Oh, and if you take out congenital anomalies as various people said we should, the rate is 0.20 for MD/hospital, 0.14 CNM/in hospital, 0.83 other/out of hospital. In which case the CNM/other ratio is 5.9 and Dr. Tuteur underestimated the risk of home birth. I'll have to go chastise her for that.
Trixie, you're being a little obtuse at this point. I was not pointing out the issues with that particular case. Goselin failed because she committed a major error - and I have never argued otherwise. I was pointing out that a blanket assertion that midwives prey upon the Amish is a fairly gross generalization, especially since the Amish actively seek them out - sometimes even in high-risk situations.
Also, I'm rather amazed that you are familar with every single Ordung among all the Amish sects. You must be far more prodigious a scholar than I. I've encountered more than a few Amish people who are open that they are directed to shun (in the conventional, not religious sense) hospitals and physicians in favor of more "natural" methods and rely upon non-physicians for their care.
@Indigo_Fire
Orac jumped right on the previous poster's erroneous assertion that Dr. Tuteur hates CNMs. He didn't question it; he rolled with it to say that Amy's "minions" should know he supports nurse practitioners. Either Orac purposefully threw out a red herring, conflated all "midwives" out of ignorance, or he credulously presumed that the accusation against Tuteur was correct. It would be nice for him if all midwives were the same, since that would supports his preconceived notion that Tuteur's a [insert pejorative] and he outlines so well why she's wrong about nurse practitioners (and her "minions" should know about it!). Again, that is only relevant if you conflate the CNM and CPM credential. Intentionally or not, that is what he does.
I do not feel like I'm "reading" too much into them. I've been reading SOB for only slightly less time than RI; Dr. Tuteur is only unequivocally against "fake" midwives, CPMs, and home birth. I do, however, feel like you're seeing the Orac & Co. team through some rose-colored glasses, giving them FAR too much benefit of the doubt.
OneOther, certainly many Amish tend towards natural treatments and have a preference for doing things that way. However, there are no religious mandates to do so. It's left up to the community and family. If you don't believe me, let's ask Dr. Donald Kraybill, recognized as the leading scholar of Anabaptist culture. He's written rather extensively on this topic, but here's a sound bite: http://www.pbs.org/wgbh/americanexperience/features/general-article/ami… " Without formal church regulations on health care, decisions are driven mostly by community and family tradition."
I'm not totally expert, but I'm married to a CNM who practiced in a hospital setting for many years.
In this particular setting (an academic tertiary care center) the relationship between the OBs and the CNMs was close and professional -- no turf battles. The CNMs earned the trust of the OBs by providing appropriate labor support, but carefully monitoring for any signs of trouble. The CNMs would consult with the OB staff as soon as there was any cause for concern. If I recall, CNMs could do some moderately risky deliveries (e.g. VBACs), but if there was anything really untoward the main responsibility for the patient was shifted to the OBs (though the CNMs would remain involved in most cases).
CNMs are not surgeons, and their training in abnormal labor and delivery, and medicine in general, is not as deep as that of OBs. However, they see a lot of labors, and they get very good at reading the situation -- in many cases their judgment and experience is well beyond that of the OB residents.
In this nearly-ideal setting, the safety record of the CNMs was excellent, because they gave first-rate care within the scope of their competence, immediately consulted whenever anything looked hinky, and were very good at spotting anomalies. It's a terrible fact that babies, and very rarely mothers, die in childbirth, but whenever things got that bad, the whole team was involved.
OneOther #220 - can you give an example of why you feel "She is extremely against the small number of CNMs who perform homebirths and is also not a fan of those in freestanding birth centers"? B/c I have met certain CNMs through SOB (regular readers) that work in freestanding birth centers and home births (one of whom I have become Facebook friends with). She has an issue with certain CNMs that practice outside of their scope and/or who have a dangerous childbirth philosophy - but that is not just for midwives, she has an issue of anyone (be it nurse, midwife or doctor) who promotes/supports dangerous home birth practices. I have been a part of conversations where I have seen Dr. Amy say that home birth / birth center birth can be a reasonably safe option for low risk women with a CNM who is practicing within her scope.
@One Other, the argument can also be made that no L+D care at all is preferable to care at the hands of a charlatan like Diane Goslin -- because the parents may be more inclined to seek qualified help should something go wrong.
Take a half hour and read the grand jury report on the three cases documented here involving Goslin, and you'll perhaps see what I mean: http://www.scribd.com/doc/176703928/Lancaster-County-Grand-Jury-Report-…
Also, Tuteur doesn't hate CNMs or homebirth. http://www.skepticalob.com/2014/01/homebirth-hater-no-but-heres-what-i-…
I honestly have a very difficult time taking what Dr. Amy and her minions say seriously. On Dr. Amy's facebook page (Fed Up with Natural Childbirth) I just read a ridiculous thread where a very articulate woman was berated for the past few days for pointing out that *according to ACOG* there IS such a thing as too high a c-section rate and we *should* be actively trying to reduce the c-section rate here in the US. These women were rabid. It was shocking, actually. They even went so far as to call her a heartless b*tch, a liar and kept grilling her on what state she got her law degree. As if that is relevant to the conversation at all. If you spend just a short bit of time with Dr. A et minions, you will see that they are staunch supporters of c-sections; elective, repeat, elective because you are afraid of labor, you name it. They support a woman's right to a c-section at all costs and will even yell, "It's a woman's choice." And, "It's none of your business." when anyone points out their very real risks. If only they would extend that same courtesy to everyone else.
You see, elective c-sections for low risk women without medical indication has a neonatal mortality rate of 1.77/1000 ( intrapartum rate unknown) which is more than triple the rate of low risk vaginal birth and more than double the risk of low risk homebirth. YET they support it and actively celebrate it.
And when they refuse to admit that unnecessary c-sections do happen and they downplay their risk, they actually put women and babies at risk. Once a woman has a c-section the chance of her *next* baby dying is doubled, tripled or even higher. The chance of uterine rupture after one c-section is just 1 out of 200. Yet, if a woman were to ask to Dr. Amy or any of her followers if she should get a c-section, they would not hesitate to tell her yes. Actually, many of the blog posts Dr. Amy writes or meant to terrify and guilt women into just signing up for a c-section. Read any of her posts about VBACs and you will see that. That may be all well and good for the first baby but it's not for the next or the next or the next. Dr. Amy has never ever admitted that to her readers but's a fact. That is not up for negotiation. A scarred uterus is much more dangerous for a mother and bay and then an unscarred one. Fact.
So, is this REALLY about trying to 'save' women from homebirths? If it was about saving innocent babies, then Dr. A et minions would also be actively trying to reduce the c-section rate. After all, ACOG just released a statement that this needs to be done. I have a different interpretation of their stance, however. They remind me very much pro-lifers. It's all about the poor innocent babies. But where is the logic? Where is the unbiased view of the truth? C-sections are much more dangerous for the mother, yet if you ask them they will tell that " A good mother would give her life for her baby's in a heartbeat," Or somethng to that effect. Does the mother really not matter? If a low risk woman chooses a homebirth she WILL avoid an unnecessary c-section. That's a certainty. And by avoiding an unnecessary c-section she is keeping her fufure children from a much increased risk of dying or brain damage and she is also preventing a myriad of future problems to herself. C-sections are dangerous for women. Has Dr. Amy ever written a post about that?
No. I propose that this is not about the "poor innocent babies". This is about shaming and stigmatizing women, just as pro-lifers do. Just something for everyone to think about.
So anon, we should just forget about babies dying preventable deaths at home birth and the only thing anyone should focus on is reducing the c-section rate?
And computer ate my nym, why are using the CDC wonderbase when we have MANA's data to use? In the CDC wonderbase "other" midwife could mean a doula or a friend who is in midwifery school. That MANA stats show the neonatal mortality rate is 0.7 The neonatal mortality rate for hospital birth is somewhere between 0.4-0.5/1000. So what is the uproar about? Even when you include intrapartum rates you are looking at a morality rate that is 2 times higher and as an absolute risk that is quite small. Not to mention, two things.
First. Dr. Amy and followers all support a mother's choice to have a c-section. If one of you signed up for one tomorrow, not one person on SOB would criticize that choice or call the mother selfish, correct? The problem is, once a woman has a c-section the mortality rate for her NEXT baby more the doubles. So why isn't that an issue? Why aren't you concerned for those "poor, innocent babies'? When a woman chooses a VBAC the mortality rate is also 2x times than if she chooses a c-section. But do you support her choice to have a VBAC? If all the women who had VBACs chose c-section instead, can you image how many babies would be saved?!! Thousands upon thousands. So why are you not trying to eradicate VBACs? Why aren't you trying to banish VBACs from hospitals? I mean.. don't you care about the babies?! One preventable death is one too many! See where I am going here? The truth is, there are benefits to VBACs as they are benefits to homebirth. And the bottom line is, if you are going to advocate for a woman to have the choice to have a maternal request c-section, you must also advocate for a woman's choice to homebirth. Unless of course you don't mind being a hypocrite.
Secondly, the MANA stats include data from 1000 unregulated, unlicensed DEMs ( direct entry midwives). Orac, did you know this? So, the MANA stats really is not indicative of the risk of homebirth with a CPM or CNM. 1000 DEMs could have very easily skewed the numbers to make them worse than they truly are. But I have yet to see anyone accept that.
And lastly, like I wrote earlier, elective c-sections with no indicated risk have a neonatal mortality of 1.77/1000 and that is for low risk women. The neonatal mortality rate for low risk women at homebirth is 0.7/1000. So it's more than 2 times as dangerous for low risk woman to sign up for a c-section because she has fears of labor pain, then it is for a low risk woman to give birth at home because she has a fear of hospitals. Question: Do you support a woman' choice to have an elective c-section?
No, doula, you should do both if you truly are concerned about teh babies. If it is really about "preventing even ONE preventable death" than you should, you must, advocate for these four things:
1. lowered c-section rate
2. no homebirth
3. no VBACs
4. no maternal request c-section
Anon, considering the educational requirements for obtaining a CPM were recently strengthened to include a high school diploma, and you can obtain certification through correspondence course, I'm not sure how DEM training standards could be appreciably lower than the CPM.
Oh great... anon/mmella/rroonie/BirthUSA is here with the same old nonsense, different user name. Again, you have NO idea if ANY deaths happened under the care of DEMs. If MANA wanted to separate deaths by caregiver, they would have. But they support all home birth, all care givers... so those are the results we have.
Delphine: I think it's awfully amazing that you take the viewpoint that people should be refused any level of care because that "may" (you don't offer any suggestions as to how effective this would be) be incentived to accept full hospital care. Frankly, if you really believe that, that's an awfully extreme position. That's pretty close to the argument that an addict should be refused any and all harm reduction measures in the hopes they may go to rehab. There is a lot of evidence that such things simply do not work - they merely drive individuals further into their own beliefs. On some level, that suggestion comes off less as thoughtful and more as intentionally cruel.
Doula- when are you going to start advocating for the end of all VBACs? When are you going to start advocating for a reduced c-section rate? When are you going to start advocating that maternal request c-sections with no medical need are dangerous?
So you think that no babies died under a DEMs care? So you believe that the less experience and education a midwife has, the better their mortality rates? Unlicensed and unregulated DEMs are the least experienced of all midwives yet you want to believe that the only deaths that occurred, occurred under the care of the more experienced/educated CPMs and CNMs? Ok. Got it.
Where did I state that "people should be refused any level of care" ? That isn't my argument. At all.
What I am saying is, a dyad in the hands of an incompetent like Goslin could well be better off on their own - because if the sh!t hits the fan, they may be more inclined to seek qualified help, rather than relying on the person they trusted who was clearly working well beyond the scope of her abilities.
Did you even skim the grand jury report on the three cases above? Did you see where the parents in all three cases sought Goslin for help for their dying or gravely ill newborns, and her recommendations ran the gamut from probiotics to cat nip (sic) to fennel drops, to driving to hospitals far from the nearest one, thus delaying qualified care when time means brain, to putting an apnic cyanotic newborn under a homemade "steam tent"...
Dani - Dr. Amy has pointed out on multiple occassions that the neonatal death rate in freestanding birth centers is indeed higher than that at hospitals. She is certainly less harsh on them then homebirths, but she has always been fairly clear (at least for me) that her preference for birthing is in a hospital.
I can admire her zeal in wanting to protect babies and maximize their rates of survival. However, as I said way up before, I sometimes feel like she does this as the expense of the reasons why some mothers wants to birth outside of the hospital. I also think she provides contradictory messages quite often. On one hand, she claims that she has nothing against homebirthing in general and wishes only to educate women on risks and issues. I can appreciate that. However, there are other sites out there that do just that. During my own pregnancy, I was a fan of Evidence Based Birth, which tries to break down data into a more user-friendly form without taking any sides (even though it slips sometimes). It's pretty clear that SOB isn't a site devoted to providing a balanced view - and that's perfectly fine, as long as it's honest.
My largest issue with her has long been her seeming disconnect between her insistence that she merely wishes to help more babies survive and her alleged distaste for those who oppose reproductive rights. One of the big things that keep midwifery alive is the data that says that mothers who engage midwives as opposed to doctors (in either hospital or home settings) tends to report greater satisfaction with their care, greater emotional wellbeing during and after pregnancy and a better relationship with their care provider. However, you won't find that information anywhere on SOB - even though it would certainly probably be of use to women. I can respect Amy's distaste for anti-reproductive rights supporters, but I find it interesting how often her own arguments parallel them by placing fetal survival above all else. I have often posed the question of whether it is morally wrong in any way for a mother to decide that the increased risk of neonatal death is acceptable to her if other aspects of the experience will be enhanced. In this sense, I always seem to winf up thinking that Amy unwittingly falls into what's been deemed "the cult of selflessness" when it comes to birth - that a mother should be willing to sacrifice and abandon all other desired aspects of the birth experience in order to most ensure infant survival. And I wonder if that is really the case.
(I realize the question I've raised is more of an ethical and moral one than a scientific one, so perhaps this isn't the best forum for it, but I find it an interesting one.)
anon:
And computer ate my nym, why are using the CDC wonderbase when we have MANA’s data to use? In the CDC wonderbase “other” midwife could mean a doula or a friend who is in midwifery school. That MANA stats show the neonatal mortality rate is 0.7 The neonatal mortality rate for hospital birth is somewhere between 0.4-0.5/1000. So what is the uproar about? Even when you include intrapartum rates you are looking at a morality rate that is 2 times higher and as an absolute risk that is quite small.
Many commentators already pointed out that the data from MANA doesn't amount to a scientific study, but a voluntary survey of their membership. And the rate of participation was about a 1/3. Which means their final numbers published embellished! Hence the need for better data. Dr. Orosz used the CDC database because it's the largest and more accurate. No, it doesn't replicate exactly the population from MANA's paper, but it can come close enough for comparison.
It's also the method used by Grunebaum et al. in a recent paper, which came to the same concussion: homebirth as it is practiced in the USA carries a significantly higher risk of death for the baby.
"Term neonatal deaths resulting from home births: an increasing trend"
http://www.ajog.org/article/S0002-9378%2813%2901155-1/fulltext
Grunebaum et al come to a risk 4x higher, which puts the absolute risk of losing a baby at more than 1 in 1000 birth. This is not small, by industrialized countries standards! Prospective parents deserve to have this data if they want to make a truly informed consent. But MANA had the data from their survey in 2009 already. And only disclosed it after 5 years of evading the issue and continuing to promote HB as "as safe or safer" than hospital. That is *not* respecting patient autonomy. Or even people's intelligence.
Which goes to the rest of Dr. Tuteur's rant: "I felt strongly that the more popular I became, the more likely I was to be forced out, so I quit."
If one actually reads the comments following that announcement, there's really not in the way of evidence to justify that self-assessment but plenty to suggest that she simply doesn't understand the concept of multiauthor blog, which is further attested by her comments about site traffic. Pure promotion isn't always the point.
I'll preemptively correct the typos in my comment in moderation:
"not much in the way" and "the concept of a".
anon (#237)
1. "Doula- when are you going to start advocating for the end of all VBACs?"
I don't think VBACs should be banned. Just as I don't think home births should be banned. However, I believe women deserve to make fully informed decisions in both cases. I, personally, wouldn't support a VBAC out of hospital b/c it goes against evidence based care. If a woman is a good candidate, I hope she has the option to have an in-hospital VBAC. I think it sucks that that is not always the case but I am hopeful - b/c there are people out there fighting for it - that more in-hospital support/options will be available in time.
2. " When are you going to start advocating for a reduced c-section rate? When are you going to start advocating that maternal request c-sections with no medical need are dangerous?"
As far as c-sections are concerned, I think it is fantastic that there are people and organizations out there trying to raise awareness about the risks of c-sections. It is a major surgery and I think that risks/benefits should be covered extensively. If there is truly no medical (or maternal emotional/psychological) need for a c-section, I can't say it would be something I'd support but I certainly am not going to try and ban them - just as I wouldn't try and ban home births. As long as women are aware of the true risks involved, it is their choice.
3. "So you think that no babies died under a DEMs care? So you believe that the less experience and education a midwife has, the better their mortality rates? Unlicensed and unregulated DEMs are the least experienced of all midwives yet you want to believe that the only deaths that occurred, occurred under the care of the more experienced/educated CPMs and CNMs? Ok. Got it."
I think outcomes from the Birth Center study (where it is mostly CNMs) compared to outcomes from the MANA study (where it is mostly CPMs/LMs) - even for comparing low risk only - show that out-of-hospital births attended by CNMs have a much better outcome. Total mortality for the Birth Center study is 0.87/1000.
I don't think there is any reason at all to assume that DEMs are responsible for majority of the poor outcomes. We can use the Johnson and Davis study from the British Medical Journal to illustrate this point.
The BMJ study is 100% CPMs and the outcomes are similar to that of the MANA study:
MANA study total mortality for low risk = 1.6/1000
BMJ study total mortality for low risk = 1.7/1000
MANA study total mortality for all risk = 2.1/1000
BMJ study total mortality for all risk = 2.0/1000
Maybe...just maybe...women who don't chose to have a VBAC...have actually done some research:
http://www.mayoclinic.org/tests-procedures/vbac/in-depth/vbac/art-20044…
VBAC: Insight from a Mayo Clinic specialist
Wonder if you're a good candidate for VBAC? If the benefits of VBAC outweigh the risks? The answer might be up to you. Here's help weighing the pros and cons.
By Mayo Clinic Staff
Years ago, a C-section ended any hope of future vaginal deliveries. Today, however, many women are candidates for vaginal birth after cesarean (VBAC). Still, the choice to pursue VBAC or schedule a repeat C-section can be tough.
Here's insight from Roger W. Harms, M.D., an obstetrician at Mayo Clinic, Rochester, Minn., and medical editor-in-chief of MayoClinic.com.
Why would a woman consider VBAC?
The risks associated with a vaginal delivery are lower than the risks associated with a C-section overall — as long as you can deliver the baby at a facility equipped to handle a C-section in case of emergency — and the recovery time is faster. VBAC might also be appealing if you have an emotional investment in a vaginal delivery or a desire to experience natural childbirth.
It's also important to consider future pregnancies. If you've had one C-section and you're certain this is your last delivery, the difference in risk between VBAC and a second C-section is probably minimal. However, if you're planning more pregnancies in the future, VBAC becomes a better option with each subsequent delivery.
What are the risks of VBAC?
For about 25 percent of women who attempt VBAC, labor ends in a repeat C-section. This is known as a failed trial of labor after cesarean.
If you must have a repeat C-section after labor has begun, you face a slightly higher risk of C-section complications, such as a uterine infection. The most concerning risk of VBAC, however, is uterine rupture — when the baby breaks through the wall of the uterus into the mother's abdominal cavity.
If your uterus ruptures, an emergency C-section is needed to prevent life-threatening complications, including heavy bleeding and infection for the mother and brain damage for the baby. In some cases, the uterus might need to be removed (hysterectomy) to stop the bleeding. If your uterus is removed, you won't be able to get pregnant again.
Can you put the risk of uterine rupture into perspective?
Uterine rupture is rare, affecting fewer than 1 out of 100 women who've had a prior low transverse uterine incision — the most common type for a C-section. Still, it's possible. And naturally, the risk of uterine rupture causes concern.
If you're considering VBAC, what's important is to make sure that the facility where you'll deliver the baby is ready to deal with that complication. You'll need staff immediately available to provide emergency care.
My Body-My Uterus-My Baby-My Choice
Wow! So many comments in such a short time. Who the hell cares if the woman chooses the hospital or the home? I thought a Pro-Choice mentality meant as much. Some need to get off their high-horse and realize they won't be able to save all of humanity. Thanks for the great laugh.
At this point, I doubt Orac is going to step up and start addressing the comments where numerous issues were pointed out about the kerfluffle/Jamie Bernstein's posts. I'm assuming - unless I hear otherwise from him - that it's because he doesn't know how to respond or how to defend Jamie b/c it's clear how bad her two posts were, as so many have pointed out now on GP, here, on Facebook, etc.
I am happy that he at least admits that home birth is risky. As he said "Be that as it may, for low risk pregnancies, the MANA death rate of 1.61 per 1000 is 4.2 times higher than the estimate provided by Dr. Amy from the CDC database of 0.38 per 1000. If we use my quick and dirty estimate of 0.5 per 1000, then that’s 3.2 times higher. Both of these numbers are within the range of what previous data have shown. For example, a meta-analysis from 2010 concluded that planned home births were associated with a tripling of the neonatal mortality rate. That’s, as I would put it, plenty bad, man."
It's one more person using their platform to inform others about the risks of home birth. Which is awesome.
I regret the error and apologize for it sincerely.
But why then did she say:
Because she was replying to these points, raised by Jamie B:
And she doesn't seem too shy to have said, "I clearly stated exactly what I was doing, fool."
Link to where the whole exchange occurred, in comments:
http://groundedparents.com/2014/02/26/guest-post-homebirth-safety-and-r…
What am I missing?
Anon -
First, I would like to point out that the 1.77/1000 figure you quote comes from a study published by Macdorman et. al. in the journal "Birth" which specifically promotes natural child birth practices. The study has been criticized because Macdorman uses birth certificate data to determine that there was "no indicated risk" associated with the cesarean, and this is generally very inconsistently and/or inaccurately recorded on birth certificates. Ironically, Macdorman herself argued recently that we can't use CDC data to compare to MANA stats because the CDC uses birth certificate data, even though birth attendant is recorded very accurately, especially when compared to indication for c-section.
Other studies find rates of neonatal mortality for elective c-section as low as 0.1/1000 - see this paper for a few citations:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2475575/#R2 This paper also points out that while neonatal mortality may be higher for elective c-sections by some studies, overall perinatal mortality may actually be lower because of the resulting decrease in rate of stillbirth with an increase in cesarean delivery. And so the plot thickens...
Second of all, I don't think the point is to ban all things that carry a higher risk. The point is informed consent. VBACs should not be banned, but women should be informed of the risk of catastrophic uterine rupture, given stats, consequences etc, and factors that make their success in TOLAC more/less likely, and offered professional judgement on the best course of action.
Women who are told that homebirth is "as safe or safer" than hospital birth are being lied to. Therefore, they cannot give informed consent. Women who are told that delivering at home in high risk situations is appropriate midwifery care are being lied to. Therefore, they cannot make informed decisions.
As for CPMs vs DEMs, we just witnessed a CPM ask for advice on facebook on how to manage care in real time when her >42 week client had zero amniotic fluid on u/s. The answer is hospital + delivery now or very likely dead baby, but instead she hung out for a day and the baby died. ANYONE delivering babies should know how to handle this. ANYONE who doesn't should not be allowed to deliver babies. Maybe there are good CPMs out there. But hiring a CPM s rolling the dice, and that is not fair to women or babies.
MANA has been using its already skewed "stats" to say that homebirth is "just as safe" when actually, that's not what the data says. That is what all the "kerfuffle" is about, ultimately.
Sorry for the obstetrics talk, Orac, but you kind of brought it on yourself.
Oh, I know how quite well to respond, as all but one of the criticisms I've seen are pretty darned lame, and even the one that's not lame doesn't invalidate my criticism. I have simply chosen not to respond since last night because, as I told one of you earlier elsewhere: (1) I always prioritize producing fresh content (which is what I was doing last night and early this morning) over arguing over published posts, particularly when the criticisms have grown repetitive and haven't become more convincing with repetition; (2) I always prioritize responding to comments by people about whom I've blogged (David Lauser, the husband of Liza Cozad, a patient of Stanislaw Burzynski, appeared in another comment thread earlier); and (3) I have a demanding day job that I will likely be at for another couple of hours today, after which I will be tired, still have to get dinner, after which I will be quite unlikely to be in the proper mood to spar with Dr. Amy's shills and minions (again, that's an in-joke, for those of you waiting to be outraged).
Athough you never know...if I sit back with a nice glass of wine or single malt scotch later I might change my mind. But probably not. So I wouldn't expect me to be back until Saturday.
Truth be told, I've already spent far more time and posted far more comments after this post than I've done after any other post that I can remember in quite a while. Arguing in the comments with commenters is not how I usually roll, particularly not at the expense of time that I could use to produce new posts. I did, however, read Amy's response and have one word for you all (and her) about it: Rashomon.
I see it.
But I don't see any conflation -- or, indeed, any mention -- of CPMs, or any indications of a failure to grasp the woo inherent in the credential.
Do you?
In the event that's not a rhetorical question, the answer is "No."
...
My turn?
I've never been good at this kind of game. I have trouble thinking of completely random, fearful conjectures that are original enough. But what the hell. I'll give it a go:
Is Doula Dani made of cottage cheese? Or an NSA employee? Or a visitor from another dimension?
Ohhai birthusa. Well, first TFB isn't all that compelling, let's not lie. And holy fuck are you ever annoying. Here I'd suggest reading this:
http://www.sciencebasedmedicine.org/does-c-section-increase-the-rate-of…
Wait, wait, wait. No, I don't, because I wasn't in error.
Those words aren't from the post in which she made the comparison without flagging, identifying, revealing or explaining that she was comparing high-and-low-risk homebirths to exclusively low-risk hospital births.
Which is a misrepresentation.
A person who advertises her strengths thusly...
...should not be playing sneaky games of that kind, then refusing to admit it.
It doesn't exactly help if he or she flies off the handle and starts calling something that reads *exactly* like honestly intended, good-faith criticism "a hatchet job" at a moment's notice, either.
And accelerating to extraneous personal attacks almost immediately is even worse than that.
The main thing is the unremarked non-equivalent comparison, though.
"It doesn’t exactly help if he or she flies off the handle and starts calling something that reads *exactly* like honestly intended, good-faith criticism “a hatchet job” at a moment’s notice, either."
Right. Except you are about one of 4 who thinks Jamie's criticism wasn't a hatchet job. The majority have spoken on many different forums now and they do not agree with you. Now Orac has swept in to try and defend her - which has has not helped her at all. It just makes her look even less credible, that she couldn't defend herself so she called in someone else to do so.
Two people - who are friends (Orac and Jamie) - who have their own issues with Dr. Amy, have tried to criticize Dr. Amy's post.... honestly intended, good-faith criticism?? Come on.
The heart of the matter is this.... Dr. Amy wrote her post to fight back against MANA's ridiculous press release and expose the MANA study for what it really shows: home birth in the USA is far riskier than hospital birth.
Now, it's not what Jamie Bernstein figured out with her critique, however it IS what has been exposed by Orac, Steve Novella, Brooze Orosz, Dr. Amy and others... and it's a fact worth repeating: the MANA study shows a substantial increase risk for babies born at home.
Are you addressing me?
Because again, if so, I don't think it's too pedantic to ask that responses hover somewhere that could reasonably be described as in the close vicinity of the substance of the post.
That's genuinely how it reads to me. But I'm amenable to argument, believe it or not.
It seemed to me that she plainly stated her reasons for saying what she was saying without undue nastiness or attitude. I saw very little snark, ad hominem, or other similar indicator of personal/ideological bias.
As I've already said, it's possible to argue that she's being too fair to MANA. But if I myself were going to do so, since she clearly, explicitly stipulated that she was speaking only about that one study and what she was saying about it was appropriately limited in tone, I'd assume the disagreement was honest until it was proven otherwise.
How do you arrive at "hatchet-job"?
Wicked internet fairies have now twice mysteriously caused the same post to vanish while it was somewhere in transit between the little box in which I tended and nurtured it from a seedling and the rolling plains and diving dells of the f'ing thread.
Why is that?
Just to be crystal clear:
I have no disagreement at all with the above. It's the trip from there to hatchet job that I'm not seeing.
Also, btw, Orac's post didn't read to me like an attack on Dr. Tuteur and didn't contain any off-sides, erroneous or otherwise culpable content at all, as far as I can see.
So examples there would be good, too.
Examples from Jamie Bernsteins post:
"She then points out that OMGZ YOU GUYS THAT’S A 5.5X INCREASE IN BABY DEATHS!"
"Ok ok ok, but even assuming that Dr. Tuteur screwed up some of the basic math here"
"Dr. Amy Tuteur was less “focusing on some parts of the study while downplaying others” and more just a sloppy and unscientific attempt at calculating relative risk"
She is much kinder to MANA and definitely gives MANA the benefit of the doubt, she minimizes the risk of home birth (examples: "For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low" and "In other words, we are comparing an extremely small risk to a slightly higher extremely small risk."), etc etc.... it's all pretty clear. Again, it's why MANA promoted Jamie's post: she makes Dr. Amy look bad, makes MANA look good and makes home birth look safe.
Thankfully, in Orac writing a post about all of this drama, he proved Jamie's conclusion was wrong: MANA study shows increase risk of death. And it's "plenty bad, man."
Dr. Amy wrote a response to point out issues that Jamie got wrong and why it was a "hatchet job."
No, ann, I was not addressing you with that comment. It was another person who has been anywhere and everywhere Dr Amy and the MANA stats are mentioned saying the same thing over and over again.
I also disagree that Jamie's piece constituted fair criticism. She based her argument from ignorance, was too lazy to fact check and was far softer on MANA than they deserved from anyone calling themselves a skeptic. Obviously they think her piece supported their bullshit assertion or they wouldn't have been so eager to promote it.
Is there a reason my posts went from going through moderation, to going straight through and then back through moderation? I thought it might be because I'd posted links but my last post had no links and is awaiting moderation.
@Doula Dani,
Having my own set of issues (like being up for 34 hours at the very least and nowhere near sleeping...), I didn't follow probably 2/3 of this thread but I am mildly curious: What is the url of the Dr. Amy post about the hatchet job?
I'll deduce the other urls I should follow later on but at least, I need this one.
Alain
No, ann, I was not addressing you with that comment. It was another person who has been anywhere and everywhere Dr Amy and the MANA stats are mentioned saying the same thing over and over again.
I also disagree that Jamie’s piece constituted fair criticism. She based her argument from ignorance, was too lazy to fact check and was far softer on MANA than they deserved from anyone calling themselves a skeptic. Obviously they think her piece supported their bullshit assertion or they wouldn’t have been so eager to promote it.
Alain:
http://www.skepticalob.com/2014/02/grounded-parents-does-a-hatchet-job-…
Thanks.
Alain, also worth a read:
http://www.skepticalob.com/2014/02/what-you-need-to-know-about-stats-ju…
That's the one example of snark I was referring to the first time I pointed out that I didn't see much.
It doesn't strike me as excessively mean, and if it's personally pointed in any way whatsoever, I'll be damned if I can see how or why.
It suggests that the writer thinks Dr. Tuteur is overstating her case.
And that's exactly the criticism she's making.
For reasons that she clearly states in plain view of the whole wide world where anybody who feels moved to do so can take issue with it it's wrong. And may the best argument win. Etc.
Those are her criticisms, beyond doubt and question. But they're substantive. She provides chapter and verse, when it comes to the reasoning whereby she arrived at them.
And I don't see any sign that she didn't diligently consider the issue thoroughly before reaching a conclusion.
She read the paper.
She didn't overlook any numbers in it.
The sole, exclusive cause of her only oversight in that department was that she took it for granted that Dr. Tuteur wouldn't have compared a cohort of low-risk births to a cohort of all births as if they were equivalent, without noting that she'd done so or explaining why.
And mistaken as that may have been, it's more indicative of good than it is bad will. I just don't see how to parse it any other way.
A hatchet job, per Websters, is...
I'd say it also connotes bad-faith argumentation that's wittingly deceptive or misleading, typically.
I agree that it's clear. Specific, too. But I don't see how it's overly kind, as opposed to overly fair.
In case the distinction isn't self-evident, my point is that I don't see anything in the language or content that suggests bias or partiality.
That's why it appears to me to be an honest argument, on the face of it.
Jamie is not responsible for what MANA does or does not do. Her responsibilities begin and end with making a fair, honest argument based on the best information available to her at a duly diligent standard.
Because that's the most that anyone can do. And nobody's perfect.
I think she did it. I guess that if someone shows me otherwise, I'll change my mind. But unless and until that happens:
To the extent that she and/or anyone else might be better served is she revisited the issue and revised her opinion as a result of this kerfuffle, I'm willing to stake all I have on its being the result of what Orac wrote having overcome the obstacle-course of landmines laid down by Dr. Tuteur in order to achieve that end.
Because Dr. Tuteur made herself look worse than anyone else could possibly do. Gender card? Check. (It was kind of a gender-card-wild affair, actually.) Victim card? Check. Midwifery-shill card? Check. Straw-man card? Check.
There's no cause on god's green earth that entitles the most righteous human being alive to resort to that, short of its being the immediate and only difference between an immanent, actual, instant matter of life and death.
Because short of that, it's a losing game, anyway.
I mean, there are destructive cults that hesitate to go that full-bore on so slight a cause.
I too thought he did good and well under difficult and consequential circumstances.
It's difficult to miss that no matter how many people point out the problems in Dr. Amy's analysis, the same swarm of half a dozen commenters from SOB show up and deluge the comment threads with repetition ad nauseum. Which is perhaps less absurd than their temerity in acting offended when called minions.
I read it. Or actually them, there are three.
But the first one is mostly dedicated to carrying on and on about one (1) misunderstanding that she's counting as multiple errors.
And that one (1) arose directly from Jamie B. having assumed that Dr. Tuteur wouldn't have compared unlike cohorts without noting it
So I didn't find it persuasive, for reasons I've already given.
Her other points were no better. As argument. They didn't reflect on her as poorly.
The second one fixates on this...
...as a kind of combo red-herring/straw-man object that simultaneously (supposedly) demonstrates:
(a) that she's being accused of quote-fabrication; and
(b) that Jamie B. is lazy, sloppy, and shoddy.
So. First of all, the context-unredacted version of that line is:
And:
(a) No reasonable, uninvolved person would construe that as accusing anyone of fabricating quotes. Furthermore, there's no suggestion of the kind made anywhere.
The entire goddamn piece is about how the numbers were arrived at. And any fool would infer from that context that the questions being raised are about Dr. Tuteur's approach to math and nothing else.
(b) The laziness suggestion also looks an awful lot like an example of someone being intentionally misleading.
JB read the paper and considered all the numbers in it diligently. Who cares if she did it by clicking on a link provided by Dr. Tuteur or not?
Her point in saying what she did is obviously no more or less than that she doesn't know where or how Dr. Tuteur came up with the figures she's using.
And the reason for that was that it wasn't evident. Or obvious. Or even readily deducible. Because Dr. Tuteur omitted to mention she was combining unlike cohorts, or say why.
The third one is the "Can women be skeptics?" thing.
And that's just inexcusable. So the least said, the better.
"Jamie is not responsible for what MANA does or does not do. Her responsibilities begin and end with making a fair, honest argument based on the best information available to her at a duly diligent standard."
Shouldn't it end with correcting errors that have been demonstrated to her repeatedly? Because she just dug herself in deeper in subsequent posts.
"Thankfully, in Orac writing a post about all of this drama, he proved Jamie’s conclusion was wrong: MANA study shows increase risk of death."
...and instead of railing on MANA for stating the exact opposite in its press release, he focused on some weird pettyness between himself/jamie and dr amy. That crap should be left at the door when it comes to these kinds of subjects. There are not enough people blogging about home birth risk, and to let it devolve into this is very disappointing.
I mean, you guys understand that there is a significant overlap between home birth midwives and anti-vaccination folks right? Homeopathy? reflexology? There is a lot of potential for a lot of people to get hurt without the right information. Worst of all in states like mine you don't need any education or qualifications to declare yourself a midwife and start practicing. There is no one to discipline or oversee what midwives do in more than one state. The bodies that do exist seem to have little control over if a midwife can just move somewhere else and set up shop again. There are major, major problems with out of hospital birth as it stands in the united states today. I just wish that people would treat this like any other skeptical issue instead of a women's issue or some unimportant matter. I didn't see any substantial argument against my comparing this to what skeptics would say in the event that chiropractors tried to pull the same thing- why is this an issue that is okay to toss to the side?
I wouldn't say I saw any laziness wrt fact-checking, within the stated terms of the piece. It wasn't a comprehensive review of the literature or the subject.
But it's a judgment call, to some degree. And I'm also sometimes outraged by a journalist's failure to call out some evil I can't help seeing and feeling too keenly ever to forget, for one reason or another. It's a terrible feeling. Very urgent in a this-must-not-cannot-will-not-stand! type of a way, in my experience of it.
I don't know. Play fair and play to win. That's what I say.
"Obviously they think her piece supported their bullsh[]t assertion or they wouldn’t have been so eager to promote it."
You have no idea what some of us have lost because of CPMs and their ilk, and you seem to have no compassion for loss mothers and other women preyed upon by charlatans. Where is your shame? I don't care if calling us shills or minions is an in-joke, its totally disrespectful of women who are trying to counter dangerous alt-med midwifery. I am in the middle of a legal fight with a birth center over some egregious misconduct and have connected with so many other women like me because of anti-home birth groups. There is *nothing* out there for most women who are wronged by midwives. Even if you get something done they usually pack up shop and just start delivering babies somewhere else. By publicly posting these kinds of comments you are casting a much wider net than perhaps you had originally intended. If you wanted to get at dr amy personally send an email. Don't use the very serious and real issue of out of hospital birth safety as a way for you to continue a personal issue with another blogger. You have authority as a physician and an influential writer- you can use it to be petty if you want, but its a pretty awful choice to make considering what you *could* be doing. You could be helping women who lost their babies from negligence and you've chosen not to. Shame on you, orac.
I really just can't bring myself to extend this to every post in the kerfuffle pile. I've never met or even heard of the woman before I'm not a publicist or crisis consultant or arbitration-mediator. And -- more to the point -- I'm not the boss of her, you or anyone.
So it's really not up to me to say how it should end. I'm not even sure I know what that means.
Strictly wrt to the original post on Dr. Tuteur's analysis of the paper and the paper itself:
Irrespective of whether or not I myself would have reached exactly the same conclusion the same way, I thought it was an above-board argument made in apparent good faith that did not misstate the specified facts on the defined terms.
And that's what "error" connotes to me, in the context of a journalist acknowledging error.
It's possible to be completely wrong without being in error. Or, ftm, without being at fault. Very possible. But that's a different issue. And it calls for a different approach.
But if you see anything awry in any of what I've said about anything or anybody, please let me know.
I'm for communication and a vigorous exchange of viewpoints, personally.
Hope that helps.
I guess I just want to add this one thing:
There's nothing I know or can think of that's more traumatic than the death of an infant or child.
I wouldn't know personally. But I take it as given that it requires such exceptional strength and commitment to devote your life to fighting in the trenches against the threat of it that it borders on true heroism. That never comes cheap. And I admire it. Revere, even.
That goes for Dr. Tuteur, and for anyone else to whom it applies.
I don't wish anyone ill. It's just not good for anybody to start giving themselves permission to cross certain lines as a reward for what they sacrificed/earned while fighting on others. Or for any reason.
Easier said than done, and blah, blah blah.
But still. Just saying.
Ah thanks Narad!
#274
"You have no idea what some of us have lost because of CPMs and their ilk..."
The writer's day job is attempting to save people from dying a premature death. If he's only average, he succeeds a fair part of the time.
That's a day's work in my book. I think he can very well go home have a scotch, forget work for a while and think about something pleasant.
I suspect he has more idea about suffering than he would prefer to.
MESSAGE BEGINS-----------------------------
Honestly, I've never been so glad to be from an oviparous species in all my life. Good luck to you my loyal minions, you know who you are.
Lord Draconis Zeneca, VH7ihL
Forward Mavoon of the Great Fleet, Pharmaca Magna of Terra, Hatchling Wrangler Extraordinaire
Glaxxon PharmaCOM Orbital
010000111101011110100000010101011
--------------------------------MESSAGE ENDS
The only one suggesting that Orac has been wanting to "get at dr amy personally" for years "licking his chops" is Dr. Tuteur and those who uncritically parrot her narrative.
It's funny, but I have read through many (not all, because OMG) of the comments on Dr. Amy's response post, and I have yet to come across even one that is slightly critical of her. One must assume no one has anything critical to say about her, right? After all, look at all the responses along the lines of "you're so brave, Dr. Amy!"
This, I think, explains a lot about this entire schmozzle. One of the participants has a very sensitive ego, and it's not our favorite box of blinky lights.
@ safety midwifery utah: You are a newbie here and unfortunately you haven't figured out how blogs work.
Whenever you visit an established blog, you would do well to see how the flow of information and comments work, before you wade in with comments attacking the blogger and attacking other posters here.
You've made some serious allegations, which to me, are proof positive that you haven't read the comments thoroughly. With the possible exception of one person who posted a comment in favor of home births with lay midwifes, no one has posted any comments that agree with her.
Now, we have the issue of Orac using the word "kefuffle" which started a major discussion about some imaginary hidden meaning and Orac referring to "shills and minions" which triggered another inane discussion by absolute strangers to this blog, who are somehow convinced that the mere mention of shills and minions on this blog are demeaning and/or some sort of secret buzz phrase.
I appreciate that you are concerned about the safe care of pregnant women and their babies, but you are preaching to the choir here (and on Dr. Amy's blog). You and your colleagues need to start posting cogent comments about safe care of women and infants, on each and every alternative medicine blog, every quack medicine blog and mainstream medicine blogs whenever home births attended by lay midwifes, are mentioned.
However you calculate it, the numbers already skew overly favorably in the direction of homebirth safety for the simple reason that no one here seems to be picking up on: In cases where the homebirth was going badly and a transfer occurred too late to save the baby, as long as the baby *technically* dies in the hospital, it is counted as a hospital death, not a homebirth death. So whatever fractional exactitude you want to argue about .4 or. .5 is already likely offset by this glaring "freebie" to the homebirth safety statistics.
Thank you for writing this. I read Jamie's original blog entry and her followup and was really surprised by how much she was attacked for it, because it seemed like a well balanced and considered discussion to me. As a mother (and skeptic) who chose to do a home birth during the years of this study, I wondered if I was just biased towards thinking Jaime's blog was well-balanced because I hold a more favorable position towards home birth. I'm really happy to see skeptics who have the necessary background to really evaluate this issue, such as statisticians and MDs, doing so because it seems like nearly every study on home birth has a strong bias in one direction or the other.
I made the informed decision to have a home birth after having reviewed a lot of the published literature at the time on it (I do have a background in biology). At the time, I felt the published studies generally indicated that for low risk women such as myself, home birth was just as safe as hospital birth, but with fewer interventions. Given the latest data you and Jaime presented, I don't think I really support home birth anymore. (I do think home birth supporters raise some legitimate concerns about hospital births which have only barely been addressed, but that is really a different topic of conversation.) I find Dr. Amy's attacks really kind of sad and a little amusing, because I think presenting the data in a clear and fair manner is the best argument a skeptic can make for their position (or else they probably shouldn't be holding that position). But then, I suppose Dr. Amy makes clear how little she believes in the ability of women to make intelligent and informed decisions, so maybe this shouldn't be all that surprising.
The digression into the Amish, which accounted for 4.8% of the comments when I counted a few hours ago, also seemed oddly misplaced.
Lord Draconis, you are indeed fortunate that you are an oviparous species, responsible only for the new fledgling shills and minions.
This shill has been busy engaging the flying monkey squad on a number of other sites. It is a dirty job, (avoiding the monkey sh!t), but I do it willingly for the establishment of The New World Order.
Jake posted a few comments at the Bot and her Spam on this blog. *Someone else* posted a comment at the bot...and several at Jake:
http://www.forbes.com/sites/nickmorgan/2014/03/13/what-public-speaking-…
@ Narad: My head is reeling and my brain has turned to mush after reading the many comments and the interpretations of those comments.
@lilady: While it's true that very few people here posted in defense of homebirth and lay midwives, an allegation I've seen repeated many times is that Dr Amy mislead her readers by comparing a bunch of both low risk and high risk homebirths with a cohort of low risk homebirths alone.
I've already wrote a comment why this is, in fact, the right comparison: because MANA lies to pregnant women that they are not high risk, just experiencing "a variation of normal". Yet when things go south, those not high risk women should be excluded from the stats?
I understand why MANA wants it both ways. It's the sudden scientific rigour of many of the commentors here that I cannot understand. Sure, it'll be more interesting to the science to compare like with like. And what purpose does it serve when homebirth midwives keep insisting that they only take low risk patients? What's wrong with taking them to their word to reveal what they are doing? The stakes are too high to play science here.
For the life of me, I cannot understand why most of the commenters here brush safety and reality away in order to be fair to those who were unfair from the start - and their patients paid the price. It certainly looks like it's all a big scientific experiment for the majority here. I can see where Safer Midwifery comes from.
Can you explain it to me? Why is it so important to compare like with like when lay midwives insist that everyone they take is "like"?
After 5 of the 222 breech babies in their "study" died, MANA still hasn't made any recommendations like, precluding women with breech babies from becoming lay midwives' patients. Would someone explain to me why we should exclude breech as high risk from homebirth stats?
Thanks very much for this post Orac and for shining a light on the incredibly shoddy and misleading PR job MANA did promoting their survey. Given that the survey had such a low response rate and that undoubtedly many of the bad outcomes were simply not reported, it reveals the parlous state of homebirth in the US. I hope that with major bloggers like you revealing the dishonesty and dangerous practices of CPMs and other lay midwives, awareness is raised across the broader Skeptical community and action is taken to protect babies and mothers from homebirth quacks.
Amazed: I suggest you look at my comment at # 93. Did you or any poster here, offer up any of my arguments against home births attended by lay midwifes...or were you too busy critiquing Orac's words and phrases.
You do have to have an understanding and the knowledge to convey to women who are contemplating home births, if you want to be effective advocates for safe births attended by CNMs and doctors, in birthing centers close to, or preferably, within the confines of a hospital.
P.S. I do peruse Dr. Amy's blog occasionally and I've posted one or two comments on her blog.
Sigh.
I'll try explaining this once more, in short declarative sentences:
The point is that she didn't say that was what she was doing or why she was doing it.
Absent that, the standing presumption on the reader's part would be that she was doing it the usual way.
But she wasn't.
So it's misleading.
And the reason that matters is:
It's the reason Dr. Tuteur appeared to Jamie Bernstein to be overstating the statistical risk.
It was therefore entirely Dr. Tuteur's own fault that Jamie Bernstein had difficulty with her numbers.
But rather than explaining and correcting the misunderstanding in a responsible manner -- as a person dedicated to educating and informing the public might reasonably be expected to do -- she went nuts and began hurling personal insults at all and sundry, while congratulating herself for her manifold virtues and splendors.
That's unseemly.
@ann, there was a reason I addressed this post to lilady. And since you've been so kind to reply, I'll give you that reason: she wasn't one of the commentors I was referring to, so I figured she might actually explain things to me.
Keep defending Jamie's laziness. Keep equaling a guru statistician to a lay reader with no more obligation to put in the massive effort to look two posts above the one she was criticizing. Keep insisting that (actually) low risk hospital birth should be compared to low risk (when it suites homebirth midwives) homebirth. I still hope lilady will take time to explain to me why her fellow commentors think it's so much important to know what dream homebirth looks like than what actual homebirth does.
@Amazed --
I haven't done any of those things. However, for the sake of the exercise:
Assessed against every conventional standard for due diligence in, journalism that I can think of, she was not lazy.
That seems like the appropriate standard to me.
But if someone points me to something she irresponsibly omitted to do, I'll change my mind.
No reader can read something that isn't there, irrespective of credentials, background and orientation.
And neither statisticians nor journalists are under any obligation to go looking elsewhere for the pertinent, essential explanatory details that a writer left out.
On the contrary, the writer has an obligation to include them.
Don't midwifery-shill me.
Also, can you read?
I said explicitly in the post you're replying to that the point is not -- N-O-T, "not" -- that she should have used a different comparison, but that she should have noted that she wasn't using the standard, default-assumption comparison.
Just got through all the comments. Correct me if I'm wrong, but the entire rationale for dr. amy's faulty comparison is essentially "they are dishonest so we should be dishonest too."
Is there some reason why she couldn't make an accurate comparison of the groups then explain further in that same post why those numbers are probably even higher?
Nutshell - you mean like when Dr. Amy wrote this:
"MANA and homebirth midwives have been lobbying extensively for a scope of practice that includes breech, twins, VBAC, etc. Now they want to exclude those same births from their statistics. Even then, the MANA death rate is 4.2X higher than hospital birth. So even when homebirth midwives stick to low risk patients, homebirth has a death rate 320% higher than comparable risk hospital birth."
Yes, but without making (not to mention highlighting) the inaccurate comparison.
Doula Dani --
That not only doesn't explain what she did -- ie, how she came up with the 450 percent figure.-- it suggests that she wouldn't be doing it.
Exactly for the reasons nutshell says. It's something they're wrong to do.
It compares ALL hospital midwife attended births to ALL home midwife attended births. BOTH include some high risk pregnancies though BOTH are mostly low risk.
Oops.
Wrong figure, sorry.
What I meant was: She's (rightly) criticizing them for wanting to exclude unfavorable statistics from one side of the equation.
That suggests she herself wouldn't do it.
The "inaccurate comparison" is not inaccurate. As I said above: It compares ALL hospital midwife attended births to ALL home midwife attended births. BOTH include some high risk pregnancies though BOTH are mostly low risk. That comparison = 450% increase, which is what she highlighted.
Right. But there was no misunderstanding or conflict about that particular figure.
Ann - she is criticizing them b/c MANA wants it both ways. They don't want home birth midwives to be limited to only low risk pregnancies and yet, when the data shows that higher risk pregnancies are ridiculously dangerous outside of the hospital, MANA wants people to ignore it and exclude those numbers from the data. All those moms who were told "don't worry, you are low risk, this is just a variation of normal" like my friend, Sara, was told by her midwives about her breech baby (who ended up dying) are just having the deaths of their babies swept right under the rug by MANA.
Um, that's not what her post says.
@Amazed (and frankly anyone who is here) - I've not commented so far in this thread. Until Orac had posted this article I had never read anything written by either Dr. Amy Tuteur or Jamie Bernstein to my knowledge, so I don't really have a horse in this race.
First off, regardless of any factual errors or misunderstanding of how Dr. Amy derived her numbers by Jamie, I did not find her piece disrespectful. All the language above about 'hatchet-jobs' seems quite out of place, especially as there did not appear to malice behind the intent of the article.
On the other hand I found Dr. Amy's rebuttal harsh beyond anything that was necessary and really out of line. All she needed to do was correct what misunderstandings Jamie might have had about how the numbers were obtained. If Dr. Amy did not provide details enough about what cohorts she was comparing and what assumptions she made such that a person using reasonable assumptions might reproduce them then that is her problem. How can you truly understand what Dr. Amy wrote if you don't know what she is really comparing?
As for the continuing issue of whether to compare low-risk home-birth or high-risk home-birth to hospital births. I don't think the issue is nearly as clear cut as you think. As MANA is self-reported there is considerable room for dishonesty in accessing risk, but I see no evidence for what fraction were not correctly accessed: 10%? 50% 80%? It seems likely that comparing low-risk home-birth to low-risk hospital is just as incorrect as comparing high-risk home-birth to low-risk hospital. One can make an assumption, but this really should be stated. If anything they will give you upper and lower bounds on the risk between home-birth and hospital birth. In both cases home-birth does not come out looking good.
nutshell - when you pull from the CDC Wonder Database, you can separate by care provider and location. For hospital births, you see MD outcomes and CNM outcomes. She uses the CNM outcomes, which includes MOSTLY low risk and compares to the MANA study. MANA study is separated into two groups: low risk and all risk. She highlights the comparison from hospital midwife to all risk at home.
For the hospital data there really is no way to completely filter out all high risk pregnancies... so high risk pregnancies like VBACs, pre-e, GDM, etc that any hospital midwives attend as the primary care giver (even with OB back-up) will be included in the hospital numbers for midwives.
Correct that it is not noted in Dr. Amy's post. That is b/c hospital midwives see MOSTLY low risk women. Just as the MANA study is MOSTLY low risk women in the all risk numbers.
I understand. She's right to criticize them for that.
But that doesn't mean she's right to criticize Jamie Bernstein for not having psychically intuited that it was her justification for comparing a cohort of low-risk-only hospital births to the cohort of low and high-risk homebirths without explanation elsewhere.
And there's nothing that would mean she was right to criticize Jamie Bernstein in some of the terms and on some of the grounds that she did.
@stewartt1982: the issue is absolutely clear cut. Which part of "we take only low risk women", "breech/postdate/twins/whatever you're having isn't a low risk, it's just a variation of normal!" and "but breech/postdates/twins/whatever ended up in death was high risk, so it shouldn't be included in homebirth stats" isn't clear cut?
What about lying to your clients isn't clear cut? How can it be excused and even endorsed by being sooo fair to actually refuse to include all those women who just fell on the wrong side of stats in those same stats?
FWIW, for the purposes of ascertaining reliable, representative, clear-cut statistical truths, I think the material is probably fully self-defeating.
Those things aren't in the paper. And she was analyzing the paper.
I know there's a reason you're not talking to me. But there's none for my not talking to you. So I am.
Ann - Jamie simply could have asked Dr Amy why she compared the numbers the way she did.
Jamie's piece is an attack on Dr Amy. She insinuated that Dr Amy fabricated quotes, twists around data, etc. Did she think Dr Amy would just let it go? Of course not. GP posted that as click bait and to get back at Dr Amy for what she previously wrote about Chris Breechen (from GP).
Late to the party, but one thing I am still wondering about is why the criticism of being "confused" and "wading through" the data is not directed at MANA, who deliberately published confusing analysis, but at a third party's analysis of MANA's analysis.
@amazed - Please don't put words in my mouth. I'm sorry to be harsh, but I don't think I said anything to get yelled at.
Where did I excuse midwives lying to their clients, or labeling high risk patients as low risk because they didn't die. It is wrong, and should be rightfully condemned. Nor am I trying to defend MANA or their statistics.
What I am writing is that one doesn't know the rates at which midwives are lying (if I missed a source, please let me know). In that case an assumption is needed. Ones assumptions and rational have to be made clearly in science. When this is not done it can easily lead to unnecessary confusion (and in this case a lot of unnecessary vitriol) as we see here.
Ann – Jamie simply could have asked Dr Amy why she compared the numbers the way she did.
When a professional publishes his or her authoritative opinion on a subject, the presumption is that all the pertinent factors and circumstances underlying it have been included.
That's a very basic obligation.
When something is obscure, unclear, or missing from the piece, "Why didn't you ask me?" is not a defense.
I mean, what if everybody started using that standard? Global Warming denialists, for example. Let's say I criticized Anthony Watts for comparing the rates of warming between 1989 and 1998 with the rates of warming between 1999 and 2008, without mentioning that since 1998 was an El Nino year, temperatures were additionally elevated during it.
Would he be justified to reply: "Why didn't you ask me? I would have told you it was because the IPCC did x, y and z."
If he's not, nobody is.
@stewartt1982: You didn't say anything to get yelled at and I didn't yell at you. I am sorry if it looked this way. I was simply asking a question. I don't think I used capital letters or something.
@ann: Now that you're no longer ignoring the problem with low risk and "low risk", I do think we can start a conversation.
Jamie's post was published on February, 26th. That's what Dr Tuteur's site looked like at the time she wrote her piece:
http://www.skepticalob.com/page/6
The piece where she cites her numbers is on the very same page as the one where she explains how she arrived at them - and had been there since February, 3rd. It was there while Jamie was writing her piece. You think she was not obliged to look at it. I think she was sloppy for not looking at it before insiniating that Dr Tuteur was a liar. We'll bever see each other eye to eye but I don't have a big problem with that. Dr Tuteur is a tough lady and she can take much more. What really matters is that the numbers show a great increase in the relative risk - something that disturbed Orac, Dr Amy, and Dr Grunebaum, all of whom have knowledge in medicine. In the light of this, I am not too bothered by the fact that a self-proclaimed guru statistician finds an increase that is measured in times "slightly or negligibly bigger".
It's a critique of her published work, which is not exempt from criticism.
The only question is therefore whether the criticism was fair.
She doesn't insinuate anything about the data. She plainly states that she can't figure out how Dr. Tuteur arrived at some of her figures.
As to the fabrication:
See that bolded portion there, where she offers a possible explanation for having been unable to locate the quote, before saying she's not sure where it came from?
That clearly suggests that she assumes some such innocent explanation exists.
I don't know or care. She has no particular obligation to think about what Dr. Tuteur will or won't do, which is -- in any event -- completely beyond her control.
Sounds like a conspiracy theory.
My apologies. I meant:
As to the fabrication:
See that bolded portion there -- which, much to my dismay, I forgot to put in bold in my previous post -- where she offers a possible explanation for having been unable to locate the quote, before saying she’s not sure where it came from?
That clearly suggests that she assumes some such innocent explanation exists
Dammit.
Apologies again.
I don't understand what I'm doing wrong. I'll go figure it out.
@Amazed
Sorry that I misunderstood.
I took your questions to be accusatory (perhaps 'yelling' was an incorrect word in the previous post) that I somehow supported them (which I don't).
I'm off anyway as I don't have much to bring to the table other than my gut reaction to the articles and comments.
^^That bolded portion.
I'm so sorry for being a stupid thread-space eater.
Damn.
I was sitting here thinking about how I would try to explain why Amy's comparison was so dubious from a scientific standpoint. I was a few dozen words into a comment that probably would have taken my usual hundreds of words to explain, because logorrhea is how Orac rolls too often, and then I see your comment. Here you are, boiling it down to its essence in a single sentence. It was as though a lightbulb went off in my head, and I realized that, if neither Amy nor her more vociferous minions can accept that this is the case, then I really can't help them understand, and spending a half hour writing a long post answering everything point by point is time that could be better spent on the posts I need to write for Monday here and at SBM and, perhaps, bringing up other points where I might be able to make some people see the problems with Amy's posts.
The sad thing is, this really wasn't necessary on Dr. Amy's part to use the wrong comparison. It really wasn't. As I said before, 4.2-fold is plenty bad, and, quite frankly, given the comparison between two data sets, which in itself is questionable and whose result was only concerning because the relative risk found was so high, high enough that one can't just hand wave away the fact that two very different data sets that might not be comparable are being compared, any difference between four-fold and five-fold would be of questionable significance anyway. If she hadn't made such a dubious comparison (plus write that horrible piece that brought gender into the mix), we wouldn't be having this friendly discussion, such as it is.
I note that, since my post first appeared, even Dr. Amy's most enthusiastic fans appear to have had difficulty defending this part of her post. They seem to have felt the need to twist themselves into contorted knots of justification in a doomed attempt explain her choice, which seemed to rely on unspoken assumptions that only regular Dr. Amy readers apparently know. People sometimes ask me why my posts tend to be so long, and one reason is that I don't take shortcuts and assume my readers know the background of the story or study I'm writing about or my rationale for doing an analysis the way I do. I try (although I don't always succeed) to spell it out every single time for first time readers, even if it's just to throw a link or two in, even at the risk of boring my regular readers with the repetition (and you know some of you get bored, as I get the occasional "get to the frikkin' point!" comment). It's one reason why my introductions tend to be so long (my self-absorbed navel gazing and/or random blathering about something or other that I thought to be related to my post being the other reasons).
I'll give you a for instance that has nothing to do with my objection to Amy's comparison. Amy came up with an estimate from the CDC Wonder database of 0.38 neonatal deaths per 1000 births in a hospital in low risk women. She didn't explain how she came up with that number except in the vaguest terms. Specifically, she didn't spell out the parameters she used to come up with that number. Trying to replicate that number, I wasted a fair amount of my time typing in different combinations of parameters, and I failed to do anything better than come close to Amy's number, which I considered to be enough for purposes of my discussion and therefore stopped. In the process, I felt Jaimie's pain, and the whole thing left a bad taste in my mouth. This is why I try to spell out my reasoning every time, even at the risk of being repetitive, which I definitely am at times. Later, Amy's minions castigated because I didn't happen to find Amy's video in which she demonstrated how she came up with 0.38? It is not up to the reader to have to look for additional posts explaining how a blogger got her results, nor is the reader in any way obligated to contact the blogger to ask. It is the blogger's responsibility to make it clear up front and to go back and put in links to later posts if further explanation was requested and granted in additional posts. Let's just put it this way: If I wrote a crappy analysis, and someone wrote a blog post deconstructing it, my reaction would not—I repeat, would not—be to whine that the blogger didn't contact me to ask me about how I did things. My reaction would be (and has been, actually) to look at myself, be hard on myself, and vow never to let this sort of thing happen again, if at all possible.
Had there been a link to that video added to Amy's original blog on the topic, that whole section in my post about my not being able to replicate her estimate would never have been written. Clearly, it was an issue, even among Amy's fans, because Amy even said in her introduction to the video that people had asked and there were still questions, not to mention that she felt obligated to do the video in the first place. So would it have been so difficult to add the link to her original post on the topic? No. Amy didn't, though, and that was sloppy. Similarly, the reason for her comparing to the MANA overall mortality rate appeared to have been assumed based on prior blog posts and/or discussions in the comments. I still don't consider the reasoning to be valid, but for the sake of argument let's say it was. Would it have been so difficult to explain it again or to provide a couple of links to previous posts explaining it? No, it would not, and not doing so was sloppy. Note that I also complained about the same sort of thing in the MANA data when I pointed out that I had a hard time figuring out how they came up with the figures of 1.61 and 2.06 per 1000. Why do Amy's minions castigate MANA (quite correctly, I might add) for this sort of lack of transparency but Amy gets a pass? "nutshell's" comment zeros in to the heart of this issue like a proverbial arrow.
I'll finish by reminding readers of a certain paragraph from my post above:
Nothing in this comment thread has convinced me I was wrong in this assessment, particularly when it's two very different data sets being compared. As I've said elsewhere, often the most vicious arguments are over the smallest disagreements.
Oh, and the whole thing about my use of the word "kerfuffle" being somehow sexist or a gender-based insult? Seriously? Does anyone realize how silly that sounds?
I was never ignoring it, from the very first one of the numerous times someone on this thread made the point, my position has been exactly the same. I'm talking about something else.
SORRY. (For that being so difficult to read.)
I'm going to get out of the way and go hang my head in shame
Oh, and correct me if I'm wrong, but Dr. Amy wrote her post before the paper was actually released, correct? I've found that that is always bad practice, and I virtually never do it. I always wait until the paper is out, at least as an e-pub ahead of print.
I forgot to say:
Quote apart from there being no such insinuation in the plain English-language meaning of the words Jamie Bernstein used, it wasn't sloppy of her not to have looked at something she wasn't writing about before not writing about it.
If that's sloppy, it's sloppy of you to comment on Jamie Bernstein's post without making sure she didn't address your concerns about it somewhere else first.
If I may, I think the primary lesson here is, in two points:
1) Show your work, all of it, the first time around.
2) Expect and respect criticism, and make corrections.
The sad part is, pretty much everyone here agrees with the most important takeaway, which is that the evidence shows there clearly is danger in home births. Everything else quickly descends into useless noise.
I'd also add, although it may or may not have made a difference in this case: Don't blog about papers that haven't been published yet based only on a press release. It's never good form, at least not for a physician or scientist.
I'm curious why your findings needed to be buried amongst some very old animosity which you clearly have against Dr. Amy. Please tell me what you think about the recent death of baby Gavin Michael at the hands of an under qualified CPM who crowd sourced his treatment on FB? Is your pissing match with Dr. Amy really more important than the extremely large numbers of babies who are dying at the hands of incompetence?
The study was published online on January 30. Dr. Amy wrote the piece on January 30.
#52 Oneother, your question "The largest question I always toss about in my head is whether or not it is acceptable in some form for an expecting woman to prioritize her own experience as paramount during birth. Is the rather obvious increase in infant mortality an acceptable tradeoff to create an experience that will be more satisfying and enjoyable to the mother?" Would probably best be answered by asking a women whose baby died unnecessarily at a homebirth, if the her wonderful experience was worth the dead baby at the end.
Orac, how many babies have to die before you have any interest in this topic? It's interesting how you seem to care so much about immunizing children to save human life after they're born, but don't care if they make it out of their mother's alive to begin with. You somehow don't seem to care if an extra 20 babies a year in the US die at homebirths, but are really concerned about the 200 or so newborns who die of whooping cough every year in the US. I just don't get it! If homebirth gets more popular and 200 extra babies die will you care then?
Now that the business of weighing in on the "kerfuffle" and critiquing various people's blogging styles, journalistic ethics and moderation policies has been explored to your satisfaction, Orac would you please give us your thoughts on how to best debunk the lies being propagated by the lay midwife community and save the lives of many precious mothers and babies?
Ann - just curious what your take is on the second post by "stats guru" Jamie Bernstein when she tried to critique the analysis by Brooke Orosz, PhD (professor of stats).
RT, If you spend any time perusing Dr, Amy's site, she actually points out that a great many women who lose babies at homebirths actually still recommend it and celebrate it - which seems to be in direct contradiction to your comment. Perhaps you should spend some time reading, perhaps?
It really is too bad that all this drama is taking away from the issue. As I've mentioned (probably 8 times now), Jamie Bernstein unfortunately did not come to the same conclusion that Orac did. She minimized the risks of home birth - which is my biggest issue that I have with what she wrote. Even when I wrote to her privately and shared info regarding intrapartum mortality rates, shared a blog post written by a CPM who took part in this MANA study in which she explained how midwives actually DID fill out information retrospectively, shared stories of two of my personal friends who had high risk pregnancies that were brushed off by their midwives who lost their babies b/c of their high risk pregnancies, etc. Clearly nothing I personally wrote to her mattered. C'est la vie. Up next came her critique of the analysis done by a stats professor..... and it not only opens up with a flat out lie about the authors of the study but then just goes on with one strawman argument after the next, *trying* to make the very good analysis by Prof Orosz look shoddy.
Someone made a comment in this second post of Jamie's: "Articles like this on “scientific analysis” in blogs by non-experts is dangerous. With all due respect, the author of this article doesn’t even have a PhD in statistics, has no medical degrees, and is certainly not an expert or “guru”"
And I couldn't agree more.
Jamie Bernstein is dangerously minimizing the risks of home birth. THAT is my main issue with Jamie Bernstein. And MANA. And all the other people out there who are minimizing the risks of home birth in the USA, adding to the preventable deaths that happen over and over and over.
I'm glad at least Orac pointed out what Jamie Bernstein didn't: death rates in the MANA study are NOT good. So I will end by saying: thank you, Orac.
RT @331 ---
Orac has a demanding day job that for most people would consume every ounce of energy. The fact this box of blinking lights manages to come home and crank out a couple thousand words of closely reasoned analysis on various other medical and scientific topics is, well, astonishing. Add to this the fact that (as he says at the very top of this post -- way, way, way up there above the comments) he has no particular expertise in obstetrics, and you have your answer.
It's entirely possible that Orac will become more interested in the homebirth issue as time goes on, but in the meantime, I think he deserves a great deal of slack. He sure doesn't give himself much.
I strongly suspect that it doesn't involve kvetching when another group of people doesn't immediately take up marching orders.
Why is a subset of Dr. Amy's minions assuming that unless one is in lockstep with them and her, then one wishes harm on mothers and infants? Us vs. them is unnecessary and counterproductive, and only seems to be coming from their side.
What is so difficult about wanting people to prove their points with honestly shown work for their math and science, in one place and NOT spread out over ten different posts and videos? Why does wanting this, which Amy did not do, suddenly conflate us with babykillers? It feels like this is the same kind of thinking that woo-y quacks bust out in defense of SCAM, except this time used in defense of something I actually agree with. (I.E. that homebirth as practice causes unnecessary deaths, and that birthing in hospital is a better choice in terms of infant survival.)
Stop making my side look bad, yo. :(
The only one engaged in any “pissing match” appears to be Dr. Tuteur.
Really? Comment after comment on here by him appears to be how unethical or not thorough enough Dr. Tuteur is. He agrees that the findings of the study are not glowing in favor of homebirth, but that wasn't Bernstein's conclusion and clearly MANA didn't find it to be that way, otherwise they wouldn't have retweeted it. If they can agree that homebirth is not safe, then why the need to discredit with personal attacks? He came out swinging and meanwhile has managed to completely derail what this talk should be all about. And if we're going to say well it's not his expertise, he's not an OB, then maybe he shouldn't have written about this to begin with. But he did and what we all really should be focusing on are those babies who are dying needlessly. Stop letting organizations like MANA sugar coat the numbers. Use all of this animosity and go after those people who are killing babies, not the ones who are trying to prevent it from happening.
There are exactly 26. Show me. Do not omit the "unethical" part or the implied intensifier.
See above.
Folks, the real enemy is out there! It's the quacks and charlatans and pushes of woo who take advantage of the sick and vulnerable. We are all on the same team. We all want to save lives through science. No one here wants to see a single baby, child or adult die because of improper care. This intramural bickering is the stupidest thing I have seen in a while, and there's a whole lot of stupid out there. Can we move on, please? Can we agree to spend our energies fighting the good fight, together as allies?
I'm waiving the white flag here.
Okay, I tried and failed to follow this comment stream. So sue me. I did notice some argument over the use of the word "kerfuffle."
The first time I noticed it being discussed online was Dr. Goldacre's blog BadScience. The discussion was that it was a cool sounding word that adequately described a certain kind of conflict which did not amount to much. Nothing to do with gender.
Today I spent the day away from home at a sewing event, which required lots of standing and I was very tired. After I arrived home we went to dinner at a neighborhood restaurant.
Due to being weary, I was not good for conversation. But dear hubby tried to engage me with news he had gathered through the day... and one of the words he used was "kerfluffle." In my very weary state I don't even remember the topic... it is just that the word stood out to me. Call it confirmation bias.
Good night. (and folks, it is Saturday evening and not even 11pm).
Scientia Est (#342) -
Hear, hear!
After watching all of the commentary for the last couple of days, it seems to me that a couple of things have been forgotten.
First: one of Dr Amy’s complaints about Jamie’s post was that it was sloppy. Jamie sent it to press with a major error, which went uncorrected for over a day because she did not have editing privileges as guest poster, and was pointed out in the comments section (i.e., not caught by Jamie).
Sure, it eventually got corrected, but does no one else have a problem with Jamie’s conclusion that “we are comparing an extremely small risk to a slightly higher extremely small risk” when her numbers were off by two orders of magnitude as originally stated? I personally don’t consider 1 in 1000 as “extremely small.” It reads to me as though she drew her conclusion from the wrong set of numbers, then tried to shrug it off as an editing error.
Second: as far as I can tell, only Ren caught this, back at comment #128: (scienceblogs.com/insolence/2014/03/13/neonatal-death-rates-after-home-births-and-a-strange-skeptic-kerfuffle/#comment-319982 )
We’re all fighting over the analysis of a paper which describes the data collection as such:
Folks can quibble over what is the right group to which to compare the MANA paper’s data set, but that won’t change the fact that the paper itself covers a self-selected survey.
Orac, how do you go from Monday’s post titled “A finger in the dike isn’t enough,” lamenting the fact that pseudoscience seems to be winning the battle in healthcare (I’m simplifying things), to--just a few days later-- supporting another website’s guest blogger defending pseudoscience ?
Sorry about the html fail.
What Ren said in #128 for those who won't cut and paste:
Everyone could have just handled all this in two simple sentences: “This was not a study. It was a survey with a low response rate and no objective way to verify the data.”
The end. No need for anything else
@ Scienca est #342
Oh, it's sadly happening regularly in the skeptic internet community, every few months. My reaction to Orac's title with the word "kerkuffle" was "oh sh!t, another one. What now?".
There are blogs I don't visit anymore because of past internet-wide kerkuffles. Either I made a fool of myself in the comments or I was put off by the pettiness of the blogger and his commenters, and subsequently decided this group of people can do without me.
My loss. Most of these blogs were high on science and/or meeting people from other ways of life.
On one hand, these heated debates are evidence that there are plenty of people over there sharing some interests, and engaging in lively debate and refinement of one's opinions.
A dissent of opinion which devolves into a shouting match is to be expected from time to time. Someone will let slip something a bit too close to a personal attack, intentionally or not, someone else will take it very personally indeed and it's all downhill from here.
On the other hand, these flamewars are eerily similar to the best religious schisms. Just saying.
It doesn't help that the skeptic community is actually a loose congregation of people with a large variety of topics of interest - sciences (too many subsets to count), medicine, religion (including lack of), ethics, social discriminations of all colors (and genders), and for the vintage-minded, UFOs (debunking of)...
So every now and then, someone will insist that his (her) pet peeve is more important than someone's else pet peeve - or that he (she) is more expert at it - and insists that the other one fall back behind his banner ("Dear Muslima"...). He is well-meaning, but pouring oil on fire.
He may be right in his assessment, but one, that doesn't mean that he has the right to compel others in that they should write about; and two, even if the second blogger's pet peeves are not as important, doesn't mean they are mere trifles unworthy of spending time for.
There may actually be a lot of trans-topic overlap. By example, discriminations based on gender, race or religion tend to have very similar social mechanisms (in-group vs out-group, power plays and so forth). More on topic, homebirth and not vaccinating are both health decisions which include a lot of the naturalistic fallacy.
By fighting one type, one indirectly helps fighting the others.
I still don't understand the defence of Jamie's piece - a hatchet job indeed when she was off by 100 (which immediately made me doubt her self-stated stats guru status) and even once she correct the math she didn't revisit her conclusions as to whether that was significant or not.
But even then, from her comments it appears that the general interest from either her or Elyse (I forget which) was in looking at how two different sides could come to different conclusions about the numbers. And after reading the paper from MANA and Dr Amy's blog post the conclusion was that Dr Amy exaggerated the risk by coming up with 5.5x instead of 4x and NOT that a lobbying group for midwives who believe in magical thinking for pregnancies and childbirth was not giving out the neonatal risk at all.
MANA have been looking at the smoking lobby groups for their tactics (hey people look - smoking makes you feel good and reduces depression and anxiety!).
I'm really baffled by the skeptics that have focussed on the trivialities and not the big picture here. How is Jamie's conclusion defensible? Even here it is stated that it is a concerning risk.
Very very few skeptics regularly cover these topics and the deaths and poor decision making and outcomes of this particular subset of alt-med practitioners. It is frustrating to see that when wider attention is given skeptics spend most of their time one-upping each other on parsing the errors of the other. Once again, I would like to see how another skeptic - it doesn't even have to be Orac - would try to parse the numbers and look at the risk. Someone with enough knowledge to not divide by one hundred when they shouldn't have.
I can understand getting a risk (0.0016) and a percentage risk (0.16%) confused like that. It's a simple and easy-to-make slip, and since it's the ratio between the two numbers (0.16 and 0.04) that's important. I don't see it as significant; it seems petty to dismiss someone because they made an error like this.
It is so hilarious/obvious that no one wants to touch Jamie Bernstein's second GP post.
And no one will address the huge issue that so many if us have with what Jamie Bernstein concluded with her first GP post, which is not the same conclusion that Prof Orosz, Dr Amy, Steve Novella and Orac all came to. Bernstein is just like MANA, guilty of completely minimizing the risks of having a home birth.
@chemomo
Indeed.
Had Dr. Tuteur said that, rather than taking the battle in a different direction by maintaining that she was the personal victim of a hatchet job who had been accused of fabricating quotes -- by someone who might, in any event, be gender-disqualified for skepticism -- and then ganged up on by an (allegedly) jealous ex-colleague with an (implicit) partiality for the other side, the whole mess might never have happened.
@KarenJJ
There's nothing baffling about it. The terms of the debate were set and defined by Dr. Tuteur. We're all just following in her path and gathering the roses she strewed about her as she progressed.
Had she been willing to act like a grown-up, cop to what she contributed to the misunderstanding by headlining a dubious comparison -- (to use Orac's word) -- without explaining it, and move on to the main point, we might all be talking -- or better yet -- doing something about that.
@Doula Dani
Please see #275
Further at chemomo --
For that matter, had Dr. Tuteur taken that approach to begin with, there never would have been any debate at all.
Jamie Bernstein is the one who ended up making the point:
"The terms of the debate were set and defined by Dr. Tuteur."
Dr. Tuteur wrote a piece about the MANA study. Jamie Bernstein tried to critique the post by Dr. Tuteur and the MANA press release at the same time. She let MANA off the hook and came up with the conclusion that 1. Dr. Tuteur used the wrong comparison groups and 2. "For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low"
Dr. Tuteur, myself and many others disagree with Jamie on point #1.
Dr. Tuteur, myself, Steve Novella, Orac, and many others disagree with Jamie on point #2.
Issues were argued in the comments of GP and Dr. Tuteur argued her points on her blog as well.
Jamie Bernstein then went on to critique Prof. Orosz (a guest post on Dr. Tuteur's blog).
I don't not feel at ALL as though the "terms of the debate were set and defined by Dr. Tuteur." This public debate started with Jamie Bernstein's first post. Both Jamie Bernstein and Dr. Tuteur have willingly participated publicly and now, so has Orac.
I greatly appreciate that Orac has pointed out the flaws in the MANA study. However, the issues with both of Jamie Bernstein's pieces still stand.
No she didn't. She came to the conclusion that she didn't know where Dr. Tuteur was getting her figures.
2. “For low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth, though because we’re talking relative risk it’s still quite low”
Dr. Tuteur, myself and many others disagree with Jamie on point #1.
That's unconventional of you, but your prerogative.
She made neither of those points in her original response, although the fifth thing on her list makes a point related to #2.
Her chief emphasis is on it having been both sloppy and a hatchet job. And you're very insistent on those things as well.
If the only issue was whether or not it was accurate and/or right to say, categorically, that relative to hospital birth, the risk of homebirth was "negligible" or "quite low," (again) there wouldn't be a debate. I agree with you that it's not.
If it was whether or not Jamie Bernstein was right to say, non-categorically, that it was what the study said about low-risk births is a slightly different question.
I'd still disagree.
But since the line occurs in a paragraph beginning "Conclusions based on this one study" that's immediately followed by one that begins "Again, just to be clear, this is not a review of all the literature and is just my reading of this one study,"; she clearly states the limitations of the data; and all the numbers are right there where the world can see them, it doesn't strike me as derelict or indicative of any major failing that she said it.
It's an appropriately qualified, by-the-book post with which I disagree, basically.
Ann -
I said "She let MANA off the hook and came up with the conclusion that 1. Dr. Tuteur used the wrong comparison groups"
you said "No she didn’t. She came to the conclusion that she didn’t know where Dr. Tuteur was getting her figures."
Wrong. Jamie Bernstein said it is the wrong comparison. To quote her "Even comparing the homebirth cohort that includes high-risk births (2.1 in 1000) to the low-risk only CDC cohort (which is not a fair comparison for obvious reasons) would only result in a 5.25x increase in mortality."
ann @ 353
Please find, quote, and link the statements in Jamie’s original post which indicate she thinks the study is “weak.”
I first read Jamie’s post during the timeframe her 2-orders of magnitude “minor” editing error were still in it, and the comments section included her pleas to the editors to fix it. I read the MANA “study” three weeks before Grounded Parents posted Jamie’s review. My reaction to Jamie’s post was that she took on material outside of her general knowledge base, and didn’t bother to read up on it before passing judgment.
What I see is a person billed as “Skepchick’s resident stats junkie/guru” who concludes her criticism of another blogger as “just a sloppy and unscientific attempt” while she has sent to press a piece with a decimal vs percent error – which is a difference of 2 orders of magnitude. Exactly who is being sloppy and unscientific here?
I can relate to typos and editing issues. I’ve left typos all over the internet and in real life because I seem to be incapable of proofreading on a computer screen. But if I were asked to do a guest post on someone else’s blog, I’d get a third party to double check that all my “i”s were dotted and “t”s were crossed before sending it in.
By the way, ann: you left an “m” out of my ‘nym. I’m not a cancer patient.
What I am referring to here is this one study. That's what Jamie based her conclusion off of and what Dr. Tuteur, myself, Steve Novella and others are looking at as well. All have concluded that home birth is far riskier.... EXCEPT Jamie.
The glaring weakness in the MANA data analysis is that only 20%-30% of MANA members submitted data, and of these, not all of them submitted all their data! As Dr. Amy pointed out on Point of Inquiry, it's unlikely that anybody confabulated deaths that never happened, but we can only guess how many midwives declined to report some or all of their data because they had bad outcomes.
Krebiozen @350
All well and good as long as the person making the error is not calling someone else out as “sloppy.”
I apologize.
She doesn't say she did, and neither did I. As she states ^^right there, she gives the reasons for that opinion in her post, while stating it in the comments.
Since that where she makes the point, that's what I quoted.
But fwiw, I assume she's referring to this:
I wouldn't say that conveys the idea that it's weak, precisely. It definitely conveys the idea that it's a limited-value, non-definitive paper, though.
Dude, she doesn't conclude that "homebirth" is any degree of risky or not risky. She characterizes the statistical increase represented by a low-risk to low-risk comparison as "negligible" or "quite low."
And, no, you're not talking about that one study, or about what Steve Novella and Dr. Tuteur said about it, for the most part. You're mostly just name-checking them.
And I'm tired of repeating myself on this.
I'm in limited agreement with you. But happily, the thing we agree about is the important thing.
Apart from that, I guess that if you gain something in some way by adhering to an unyielding, Dr.-Tuteur-Right-or-Wrong, Jamie-Bernstein-Sucks line, more power to you.
But it's not for me.
ann
Thank you.
Sorry, missed this earlier.
You said that she came (and I quote) "to the conclusion Dr. Tuteur used the wrong comparison groups."
She did not. She ruled that possibility out, because, as she said in the comments:
And what would that prove to most people?
Hint:
It was not a hatchet job.
Honestly, I have a really hard time following what you write, Ann. But we disagree on Jamie's GP post. I do think it was a hatchet job. I think she wrote TWO hatchet jobs for GP: one trying to tear apart the analysis by Dr. Tuteur and second one trying to tear apart the analysis by Prof. Orosz. I think she is a lazy writer and even when faced with errors, she is resistant to make changes. The error regarding the study authors is pointed out multiple times in the comments and she has yet to make changes.
I will agree to disagree with you, Ann.
Thanks, DD!
Also, Jamie Bernstein said "purposefully" when she meant "purposely" in the line I just quoted from her.
It's not like I'm saying she's perfect.
Be well.
"I’m in limited agreement with you. But happily, the thing we agree about is the important thing."
Perfect!
I think "skeptic kerfuffle" would be a good name for a band. Or maybe a coffeehouse. Or a dessert!
Skeptic Kerfuffle, served plain, a l'Orac, or aux framboises.
There are those who are starting to refer to this dustup as the "great skeptic kerfuffle kerfuffle."
Plus I just remembered, it's already a George Harrison song.
("And he had to have them all pulled out after the Skeptic Kerfuffle." White Album, natch. It's about when he dropped acid with his dentist. Or maybe Paul's. It's been a while. )
That was mystifying. "Kerfuffle" is the veritable model of a value-neutral word. It couldn't be more stylistically typical of you.
You're a gifted and original writer, btw, Orac.
Myself, I like the word "brouhaha".
I'm also trying to bring back the word "groovy", but with limited success.
Wrong, ann: Traveling Wilburys, not the White Album.
http://somethingelsereviews.com/2012/12/04/there-was-this-funny-little-…
I was beginning to think you had misinterpreted the While Album worse than that guy not executed by the state of CA.
Side note: my 9-year old thanks you for prompting me to play it.
@Chemmomo
I identify. That record was practically my life when I was nine.
@palindrom
I, on the other hand, am trying not to be unable to stop myself from thinking "let the morningtime drop all its petals on me" on and off all day every time I pass the 59th Street Bridge.
("Life, I love you/All is groovy!/La, la, la, la, la, la/Feelin'" etc.)
@Chemmomo
Just got and appreciated your Manson reference.
I'm slow.
ann, the same 9-year old mentioned above plays Parsley, Sage, Rosemary & Thyme falling asleep at bedtime.
@ann re #376 Glad you let me know.
Dr. Amy wrote her post before the paper was actually released, correct?
I can't tell you for certain when she wrote the post, but the first post contained a link to the full text so at the very least she didn't publish on the paper until it was out.
@Chemmomo, OT, but just last week I was reading about the history of the song "Parsley, Sage, Rosemary & Thyme":
http://www.justanothertune.com/html/cambricshirt.html
LW: thanks!
And completely topical with the musical choices for my evening.
UC Davis has one of the foremost agricultural schools in the country.
An ambitious young grad student enrolled in their PhD program. He set himself the task of becoming the world's foremost expert on a single crop, figuring that this would guarantee him the fame he deserved in agronomy circles.
At first he started studying wheat, but discovered after some months that the literature on this crop was much too vast to master in a lifetime. Corn was even worse, with its many varieties; he next tried various kinds of beans, and ran into the same result.
Finally, he narrowed his work down to a relatively minor herb garnish; even for this, the task was huge, and it was going to take some time before he had a PhD he felt properly represented his talents to the world.
Meanwhile, his fiance, Rosie, was getting impatient. Because of the demands of his deep study, he had said that they could not possibly arrange to be married until after he earned his degree.
But he urged her to be patient, because it would happen:
"I will be a parsley sage, Rosemary, in time!"
You're banned from the internet.
I knew a guy that ran in agronomy circles. The farmers kept yelling at him to get out of their fields.
(Note, I gave up on this thread around comment 220, and then only read Orac’s and other regulars’ posts.)
@Orac: I’ve been reading you daily for close to a year and this is the only post where I thought you looked particularly biased (and l’ll thank you for being upfront about it). As I said from the start, I’m sure there are issues with Amy’s analysis that are debatable and should be debated, but when you write things like this:
“Had there been a link to that video added to Amy’s original blog on the topic, that whole section in my post about my not being able to replicate her estimate would never have been written. […] So would it have been so difficult to add the link to her original post on the topic? No. Amy didn’t, though, and that was sloppy.”
I get the distinct feeling that we are going away from a scientific analysis into trivial nonsense and criticism for the sake of criticism. I understand you are trying to justify yourself and Jamie, but I don’t read RI for its courses on How Blogging Should Be Done And Why Writing New Posts Instead Of Updating Old Ones Is Wrong.
And then this:
“I’d also add, although it may or may not have made a difference in this case: Don’t blog about papers that haven’t been published yet based only on a press release. It’s never good form, at least not for a physician or scientist.”
I understand what you are trying to say. But in the context of this post and your blog, this just makes you sound ridiculous. To me, you sound exactly like someone who would come here and say “you can’t discuss the case of Sarah Hershberger until she dies [and let’s all hope that does not happen] or independent analysis confirms that she is cancer-free”.
Obviously, this won’t stop me from reading your posts in the future (this type of sloppy and biased post is, as far as I can tell, the exception to an otherwise great blog).
Edouard Brière-Allard
@EBA
When I read the posts, I had the same criticism as Orac, that she should have shown her work or, failing that, added a brief explanation or link after she got so many questions about how she arrived at her numbers. It is the writer's responsibility to explain what, how and why, not the reader's responsibility to read the author's mind. Pause for a moment and ask yourself: would you allow, say, MANA to do the same thing and get the kind of pass that Dr. Tuteur is getting?
I can see why you would misunderstand Orac's point, since your analogy is not appropriate. The right analogy using Sarah Hershberger would be something along the lines of: "Don't discuss how Sarah Hershberger died until after she's actually died."
Just like you shouldn't talk about how someone died until they've died, don't talk about the presentation of study results until the study results are published (i.e., presented). You want to write about how MANA typically distorts things, fine, but don't discuss a study they did when all you have available is a press release, unless you clearly state that you are pulling your info from the press release rather than the full study.
@Todd W.
Thanks for your reply.
I agree with you that it is possible to criticize Amy for not providing all the information necessary for the lay public to reproduce her calculations, but I still feel that Orac’s criticism goes beyond that. Apparently (I have only been following Amy’s blog for a few weeks after seeing it mentioned here or at SBM), Amy’s style is to write daily posts about whatever she feels is worthy of her attention, and to discuss old posts with new ones. I don’t think that the fact that she does not blog the way you would like her to is a valid criticism. Assuming that she really does address any questions in the comments or in subsequent posts, it’s a perfectly valid style of blogging.
You are right that I would not let MANA get away with an opaque analysis, but it seemed that it was exactly what Amy was trying to avoid. That’s why Jamie’s article was so surprising to me. Jamie did a lazy analysis to criticize what was, to her, a bad analysis from Amy in order to defend her conclusion that “[f]or low-risk births the neonatal mortality rate of having a homebirth is either negligible or slightly higher than that of a hospital birth […]”. For her article, Jamie picked an angle and a level of effort/analysis that would help MANA get a free pass. Because of that, Jamie’s entire article, to me, read like an attempt to minimize the risks of homebirth with lay midwives.
I assure you that I understand Orac’s point about unpublished studies. It’s perfectly valid for him to feel that people should not comment on the results of a study before it’s published. What I’m saying is that I don’t feel the same way. While no analogy is perfect, mine was good enough. A press release about a study will often include some of the main results. When you make something public, people are free to discuss it, even if they bend the Rules of Proper Blogging About Science in order to do so.
Edouard Brière-Allard
@EBA
As evidenced by comments she apparently received shortly after putting her post up, the criticism is valid. She was not thorough enough, necessitating subsequent posts clarifying different parts of her original post. Sure, it's one style of going about blogging, but it is sloppy, and by your own words, you wouldn't let MANA get away with doing something similar. I'd hazard a guess that none of Dr. Tuteur's regulars would, either. Yet they accept it in Dr. Tuteur, perhaps because they have the back story and they know (some of) the assumptions she's making. So they give her a pass and ignore the larger picture of clear science communication. If that is indicative of Dr. Tuteur's style, I would feel uncomfortable directing people to her posts, because I could not count on them being very robust, even though her conclusions may be valid.
And like I said, that's fine, just state that that's what you're doing.
Honestly, it seems that Jamie has earned herself a free pass here b/c people are trying very hard to tear apart what Dr. Amy wrote. No one (still) will address Jamie's second post on GP. No one will address the fact that Jamie's conclusion does not match the conclusion that many other experts have come to (actual experts, not just self-proclaimed "stats junkies") including Orac, which is that the data from the MANA study shows an increase risk to babies born at home, and it is not a small little risk. The reason I keep bringing it up is b/c it's a very, very important piece of this whole puzzle.
If Orac wasn't friends with Jamie and if Orac had no history with Dr. Amy, I do not feel his article would be written the same way (I doubt he would have even written it at all) -- nor do I feel that any of his "minions" ;) would be reacting the same way, either.
I will admit that reading Jamie's article was hard for me as she does minimize the risks of home birth and let's MANA off the hook - yes, I am an SOB reader but I would have reacted the same if she had written about Steve Novella's and come up with her same conclusion. I am no doubt a biased reader on this topic b/c I feel very, very strongly about the big issues of home birth in our country. So when I read comments like this from Jamie Bernstein:
"I’m not really sure exactly where this quote came from and these numbers don’t seem to match anything in the study. My best guess is that the quote came from a press release or results summary. The stats she mentions (2.06 per 1000 risk of death for all births and 1.61 per 1000 risk of death for low-risk births) are not mentioned anywhere in the actual study, though that doesn’t mean they are not accurate."
It comes across to me that she is implying that Dr. Amy fabricated that information.... and if any other potential home birthers read that, it may leave the same impression -- and that worries me.
And again, Jamie Bernstein's conclusion and comments such as this "In other words, we are comparing an extremely small risk to a slightly higher extremely small risk" minimize the risk -- which worries me the most.
I truly feel that the motivation in Jamie Bernstein writing her two critiques for GP were not as pure and simple as just trying to provide a skeptical viewpoint. I found it was most apparent in her second GP piece.
@ Doula Dani: How about you stop perseverating about this topic and stop cross posting your multiple comments on Respectful Insolence and Dr. Amy's blog?
Haven't you and the other posters, who employ this tactic, got a life outside of the internet? Shouldn't you be posting on blogs where the lay midwifes are plying their trade and pitching their services to credulous pregnant women?
To reinforce what Todd W. stated above; I will no longer link to Dr. Amy's blog because of the drama and the repetitive school yards taunts.
lilady -
First... what have I cross posted? I cross posted "multiple comments?" Oh really? Which ones, lilady?
Second "Shouldn’t you be posting on blogs where the lay midwifes are plying their trade and pitching their services to credulous pregnant women?" -- believe me, I do. When I have the time and when I know about it, I add my thoughts.
Third - you can link and not link to whoever you want.
"I will no longer link to Dr. Amy’s blog because of the drama and the repetitive school yards taunts."
Do as you wish. I will continue to link to articles by Dr. Gorski that I love, refuting anti-vax nonsense -- even (incredibly rude) minions like you won't stop me from using a valuable viewpoint/resource to fight for a good cause.
Actually, I'd go so far as to say the same thing about Dr. Tuteur, the vitriol of her fans and their tendency to swoop into comment threads like this one if they perceive their hero has been wronged notwithstanding. I'll still use her posts when appropriate, although it won't be that often because I don't often write about the topics she does. I must admit, though, that last limerick of hers almost made me change my mind. Holy hell I'm embarrassed for her on that one.
http://www.skepticalob.com/2014/03/a-limerick-in-response-to-dr-gorski…
Honestly, this isn't about Dr. Amy for me. Yes, I read her blog. Her blog helped open my eyes to issues I did not know existed with home birth and I'll forever be grateful for that. But this, for me, is about Jamie Bernstein's posts. It is about risks of home birth being minimized and her attacking the credibility the most outspoken advocate we have for our cause.
I am not *as* active in world of fighting against anti-vax things but it's a debate I won't shy away from b/c it is something I feel passionately about.... and if Dr. Gorski's credibility were being attacked, I would defend him as best as I could. B/c I would not want anything like that to take away from his message.
I don't know why either of you spend any time writing about each other negatively. You both have such good causes to fight for and there is no need for either of you to attack each other. Save the bitterness for private correspondence or for your therapists. You should be publicly praising each other and the valuable work you are both doing to save lives.
I came back to comment b/c I was hoping that now that things had dwindled down, that those of us left could discuss without all of the derailing.
Orac, I wasn't going to mention that dreadful limerick post, but that was the deal breaker for me. Many of Dr. Amy's loyal minions have posted comments about her two back-to-back nasty posts.
I'm obviously not as nice as you. :-)
And, yeah, if I wasn't done before, I am now.
It really is a bit of a cult of personality over there, isn't it, though? Sigh...
If you understand who Amy's commenters are, you'll understand the cult of personality. Many mothers whose babies died at homebirth or in a non-hospital affiliated birth center. Many clinicians (MDs, nurses and CNMs) who've had to watch babies die or suffer severe lifelong injury after midwives dump the mothers at the ER when homebirths go wrong.
The thing is, as much of a nutjob as Amy can be and as sloppy as she can be, she's the only person going balls to the wall on this issue. She's been screaming about the increased risk for years and recently information has been coming out that demonstrates she's right (Grunebaum's study, the Oregon homebirth stats presented to the state legislature by Judith Rooks, MANA's stats). When parents lose a baby at homebirth, they go to Amy because there's pretty much no one else to go to. The states aren't regulating around this issue and lawyers won't take midwife cases because they carry no insurance and have no assets.
I wish other people would take up this cause because right now Amy's the only person beating the drum and it's easy to dismiss her as a nasty, crazy bitch. Which she kind of is. But she's right about homebirth and she's been willing to deal with the shit that the homebirth supporters have thrown at her (including DMCA takedowns of her site), so I'll always respect her for that.
I know you say it's not really your beat, but if there's ever a slow day in the anti-vax and cancer woo worlds, there are definitely some Dr. Amy style topics that could use a heaping application of insolence. Like the low, low educational and clinical standards for Certified "Professional" Midwives, just to name some low-hanging fruit: http://safermidwiferyformichigan.blogspot.jp/2012/09/cpm-education-bar-…
Not to defend poor professional standards, but how financially viable are CNM-staffed midwifery practices. I was initially reminded of this story from a decade ago in my neck of the woods (mainly because a friend of mine – geneticist, not midwife – was part of the opposition), but it didn't seem to have any particular relevance earlier on.
Yikes.
That kind of thing really has to be clever to work.
That way, you won't leave people wondering why your second line doesn't scan, when it easily could.
___________
There once was a doctor obstetric
Who promoted herself as a skeptic
Yet when challenged on facts,
She replied with attacks,
And eventually grew apopleptic.
___________
That's not very good. But when in Rome.
I'm from Chicagoland as well, so I know Illinois definitely had (has? I don't know, I've since moved away) a problem with malpractice premiums for OB and CNMs. Just off the top of my head, I have a friend who delivered with the CNM practice at GW in Washington DC so such practices are still going strong in certain areas.
But even if the financials were bleak for CNMs everywhere, that wouldn't justify the existence of a second class of midwives with totally substandard training and experience, would it?
I don't understand the last line, either. What or whom is she tossing?
I certainly hope this doesn't turn out to be like that time I saw a girl who looked a lot like her up on Choctaw Ridge, when she and Billie Joe was throwin' somethin' off the Tallahatchie Bridge.
Because I've never been able to figure that one out.
Seriously. I'm confused. Babe-mourning > exploitation of conflict > ego-salving is not a natural or sensible progression.
No, it wouldn't. I thought I was clear in explicitly disclaiming any such position. It might, however, have some explanatory power.
I don't know what ultimately happened with the U. of C., but they have a long history of dumping poor financial performers, like, say, the trauma center. (Seriously, while I haven't been in Stroger, the U. of C. is, bar none, the most unpleasant ED I've ever experienced.) The University of Illinois Medical Center's CNM program seems to be going strong, but then again, they also happily accept Medicaid for top-flight specialty care.
Nah, I'd say it puts Dr. Tuteur's clumsy effort to shame.
Sorry about that. You were clear, I just need a second cup of coffee I'm afraid.
The desire to avoid the expense of carrying malpractice insurance is surely one reason some women choose the CPM route over CNM schooling. The desire to take shortcuts is another. You can self-study your way through the educational portion of the CPM, attend a mere 40 births and you're done!
Great for the midwives' bottom line, bad for moms-to-be.
Talk about damning with faint praise. That's not a high bar to clear.
Not to take anything away from her that she properly merits, which I'm sure is plenty. I guess she must be in a lot of pain, in one way or another.
However, Orac hasn't done a damn thing wrong or deserving of rebuke.
Also, thank you!
Doula D. said:
"Still no (meaningful) responses from Orac. I keeeeep checking…."
English translation: "WAAAAAAHHH! Orac won't bow down to me!"
This comment is in regards to your response to concerns given by posters who mentioned that many women seek home births due to fears of c-sections, and to another about maternal deaths. You brush them both off as not relevant to the discussion (since your post is about a statistical discrepancy). While it may be true that your post is mostly concerning different interpretations of a study, you also mention that women who choose a home birth are doing so only because they are being misled about the risks of doing so. You don't bother to find out about whether the risks of birthing at home are greater or less for the mother, both in terms of death other, less quantifiable issues. Please take some time to find out why women are choosing home birth -- it's often after a negative experience birthing in a hospital or after a friend's negative experience. You generally support most medical care, and hospitals in general. Why? Why not research some of the issues they may have that they may also be hiding?
Anyway, here are a couple of links for you to read (you probably will just laugh them off):
http://www.reuters.com/article/2014/05/06/us-health-maternity-idUSKBN0D…
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2920649/?report=classic
From your first link:
"WHO experts said the increase in the U.S. mortality rate may be a statistical blip. Or it might be due to increased risks from obesity, diabetes and older women giving birth...
Globally, most maternal deaths are caused by severe bleeding, high blood pressure, infections and obstructed labor."
And your answer to those risks...is home birth with a doula? Really?
Truly abusive behavior by doctors (hopefully better documented than through anecdotes from "Doula V" and "Doula M") should be reported to hospitals and medical boards. The answer to that behavior is _not_ to subject patients to unnecessary risks from unqualified personnel at home births.
That first link is to a report that came through on my MedScape email notification several days ago. I thought it might come up on an anti-vaccine site...so props to Jennifer R for reviving a dead thread.
The reference point for the second article is a 60 year old article which was not published in a medical/nursing/science journal:
http://en.wikipedia.org/wiki/Ladies%27_Home_Journal
"Anyway, here are a couple of links for you to read (you probably will just laugh them off)"
Ha, ha, ha, ha.
While it doesn't have the journalistic credentials of Women's Wear Daily (really), the Ladies' Home Journal can come in handy:
"Miss Hickey: Tell us about your most recent crisis.
"Mrs. McKenzie: I had given a birthday party for fifteen children in my little living room, which is seven by eleven. The next morning my son, whose birthday it had been, broke out with the measles, so I had exposed fifteen children to measles, and I was the most unpopular mother in the neighborhood. He was quite sick, and it snowed that day. Ed took Lucy sleigh riding. Both of them fell off the sled and she broke both the bones in her arm.
"Mrs. Gould: Did she then get the measles?
"Mrs. McKenzie: She did, and so did the baby.... My main problem was being in quarantine for a month. During this time that all three had measles and Lucy had broken her arm, we got a notice from the school that her tuberculin test was positive – and that meant that one of the adults living in our home had active tuberculosis. It horrified me. I kept thinking, 'Here I sit killing my three children with tuberculosis.' But we had to wait until they were over their contagion period before we could all go in and get x-rayed.
"Miss Hickey: And the test was not correct?
"Mrs. McKenzie: She had had childhood tuberculosis, but it was well healed and she was all right. About eight of ten have had childhood tuberculosis and no one knows it.
"Mrs. Gould: It is quite common, but it is frightening when it occurs to you. Were your children quite sick with measles?
"Mrs. McKenzie: Terribly ill.
"Mrs. Gould: They had high temperatures?
"Mrs. McKenzie: My children are a great deal like my father. Anything they do, they do to extreme. They are violently ill, or they are as robust as can be. There is no in-between..."
I will start with a conflict of interest. I am a midwife. I have been a part of both hospital and home birth. I work in a practice that contains both CNMs and CPMs. We attend birth center and home birth. Our CNMs do not consider themselves superior to our CPMs and visa versa. In my community we have some wonderful bridges with doctors and hospitals in the event a home birth requires transfer. In my practice at our initial interview before we accept a patient we always make sure they are clear that a transfer of care to the OB is not a failing of the midwife or the mother but good quality care. We repeat this when risk factors present. Once a month we bring in outside trainers to provide continuing education and practice birth scenarios. We have monthly review as a practice where any patient that presents with a non absolute risk factor is discussed as to whether continuing care is appropriate. Every patient with an absolute risk factor we transfer from our care is also discussed. We consult with one another and with OBs is our community. In my practice, every birth outcome (even if they transfer to another provider at any point during care) is tracked-through MANA as well as in house. Our statistics show that our practice has safer outcomes than those published by MANA and those represented here using the wonder database. The policies we follow in our practice are one of the reasons we have such good outcomes. We have an obstetrician in our community with outcomes far worse than the wonder data or even MANA. I say this neither to condone nor condemn midwives or OBs but to illustrate that the greatest weakness in analyzing data from MANA as well as CDC data is that there are an incredible number of variables to control. With such variation from practice to practice and the reality that reporting by either the medical establishment or midwives is not always perfect, using a nationwide picture does not give patients a true understanding of the risks they are assuming when initiating care with a provider or choosing a birth location in their own community. This is why Dr. Amy can feel so abrasive not just to midwives but also to the obstetricians who act as our consults and back-up during birth. I believe that statistical outcomes for an individual practice and practitioner should be made available to patients before they initiate care and patients should understand that the overall statistics in a given practice do not and cannot guarantee a desired outcome. Yes, some midwives will not be as diligent about insisting a woman receive a recommended therapy or testing. The midwife may recommend it. She may lay out the research behind it. She may order a consult with an OB. In the end the mother must choose for herself whether she will receive recommended treatment or testing. If she refuses, a midwife must decide whether to risk the woman out of her care, which in some situations is far more nuanced than checking boxes on a form. In my own practice we've had to ask ourselves whether a woman who is noncompliant will then attempt an unassisted birth despite her risk factors. If so, do we have an ethical responsibility to the well being of both mother an baby to continue care with careful documentation of noncompliance, our consults with other providers and our attempts to facilitate a transfer of care to another provider. Some doctors will rush to intervene, perhaps unnecessarily. They may unintentionally create a situation in which ever greater and riskier interventions are needed to have a 'safe' outcome. These realities cannot be gleaned by a patient from the reports debated here. There are no easy answers. Large nationwide and even state level statistical analysis can help us refine scope of practice, absolute and non absolute risk factors for out of hospital providers as well as set in place minimum provider education requirements. (Because some people here are unaware, there are CPMs who participate in more more births than CNMs before completing their education. They may spend 5 or 6 years in training. Not all but certainly not a significant minority either. Making the assumption that a CNM program is necessarily more rigorous than all CPM programs is false.) These large statistical studies cannot decide for a woman what her birth choices should be, nor what her outcome will be no matter where or with whom she decides to birth.
t, I appreciate your contributions, but please -
Paragraph breaks are your friend. Take advantage of all they have to offer.