It's always disappointing to see a good journal fall for bad medicine, particularly when it's in your field. For example, the Journal of Clinical Oncology (affectionately referred to by its abbreviation JCO) is the official journal of the American Society of Clinical Oncology (ASCO) and probably the most read clinical journal by those involved in the clinical care of cancer patients. Just as most oncologists, surgeons, and radiation oncologists who specialize in the care of cancer patients belong to ASCO, most of them also at least peruse JCO on a regular basis because major results of large cooperative group trials are often published there. Basically, everyone wants to publish his oncology clinical trial in JCO. Getting into Clinical Cancer Research is good, but getting in JCO is great.
So when I see a study that some of you have been e-mailing and Tweeting at me in JCO, I can't help but wonder what the hell happened to peer review at the journal. I also realize that, being in the biz myself, by criticizing the peer review at JCO I might endanger my own chances of ever publishing in there given that my meatspace identity isn't exactly a particularly well-kept secret (nor is it meant to be anymore). Oh, well. It needs to be said. Earlier this week there appeared in the Early Release Articles a study by Jun J. Mao and colleagues at the University of Pennsylvania entitled Electroacupuncture Versus Gabapentin for Hot Flashes Among Breast Cancer Survivors: A Randomized Placebo-Controlled Trial. Sounds neat, right? Sounds like a head-to-head battle between every acupuncturist's version of transcutaneous electrical nerve stimulation (TENS), electroacupuncture (EA), versus gabapentin (a.k.a. Neurontin) in a battle royale to see which can alleviate hot flashes the best.
And make no mistake, hot flashes are an incredibly important problem in oncology, particularly for breast cancer patients. Patients who have breast cancer that is estrogen receptor positive, which means that the cells are responsive to estrogen, are frequently treated with drugs that block estrogen action. If a woman is postmenopausal, the usual drug used is a member of a class of drugs called aromatase inhibitors. If the woman is premenopausal, the usual drug used is Tamoxifen. In either situation, the most common—and frequently the most troubling—side effect of the drug is menopausal symptoms, mainly hot flashes. What a lot of people who aren't cancer doctors or patients don't understand is that these hot flashes can be horrible. Believe it or not, I learned this lesson with the very first patient I treated as an attending surgeon, lo these many years ago. This woman had such horrendous hot flashes from her Tamoxifen, as well as psychological symptoms, that she and her oncologist, after attempts at dose reductions and other strategies to ameliorate her symptoms, jointly decided that she couldn't take it any more. Unfortunately, for patients with hormone-responsive breast cancers, the most bang for the buck in terms of preventing recurrence comes from the hormonal therapy, at least equal to that of any chemotherapy. So the degradation of quality of life and sometimes even symptoms necessitating cessation of hormonal therapy are a major problem in oncology. Unfortunately, our existing treatments are not the greatest, which opens the door to woo such as acupuncture. Where there's woo, there's quackademic medicine to study the woo, and that's just what this study is.
Basically, this study is a bait-and-switch. I realize that I just discussed another bait-and-switch acupuncture study less than a week ago, but sometimes a doc's gotta do what a doc's gotta do.
So where's the bait and switch? In this case, it's on more levels than you think. In fact, before I dive into the story itself, let's look at the spin being put on the results. I like to call this how not to report on an acupuncture study:
Needles beat pills for treating hot flashes in breast cancer survivors, according to a new trial that compared acupuncture, "sham" acupuncture, the medication gabapentin and a placebo pill.
Interestingly, sham acupuncture came in second place for effectiveness, the researchers said.
Furthermore, the effects of acupuncture were "significant and enduring for hot flashes while gabapentin's effect only happened when a patient was taking the medication," said study first author Dr. Jun Mao, an associate professor of family medicine and community health at the University of Pennsylvania in Philadelphia.
The study was published Aug. 24 in the Journal of Clinical Oncology.
As usual, the reporting that "acupuncture beat pills for hot flashes" is a completely inaccurate assessment of what the study actually showed. The study showed nothing of the sort. Barring an incredibly strong effect, it couldn't possibly have (more on that later). Sadly, dissecting the BS attached to acupuncture studies is a rather specialized skill set; so perhaps I'm being too harsh. There were others who fell for this. When this study was presented as an abstract at the San Antonio Breast Cancer Symposium in December, similar stories were written about it. Of course, given the depth and breadth of science presented at the SABCS, it never ceases to amaze me how the press always seems to zero in on studies like this one, which tell us very little but give the appearance that acupuncture works.
Acupuncture is, of course, a theatrical placebo. Its effects are nonspecific, which is why it is such an adaptable placebo. As I joked sarcastically last time, if you believe its practitioners and adherents, acupuncture can treat almost any disease or health problem to which human beings are prone, which is why last week I could be blogging about a bait and switch study of acupuncture to treat hypertension and this week I can be writing about a bait and switch study of acupuncture to treat hot flashes caused by hormonal treatment in breast cancer patients. That's why several years ago I was writing about worthless acupuncture studies examining acupuncture for hot flashes.
This study, in fact, shares a major flaw with the one I blogged about in 2008. Specifically, it has no control group that received no treatment at all. For a study that goes on and on about placebo effects and how acupuncture provides more of a placebo effect than pills, that's a rather glaring omission. So let's look at the study design. Basically it's a four arm study, two arms of which look at electroacupuncture (EA) versus acupuncture and the other two at gabapentin versus a placebo. Interestingly in this study compared to most electroacupuncture studies, the EA is considered the "real" acupuncture and the standard acupuncture (SA) is described as the "sham," which, I have to admit, is not inappropriate, given that acupuncture is a sham and electroacupuncture is basically transcutaneous electrical nerve stimulation rebranded as the sham that is acupuncture. (We all know that those ancient Chinese must have had access to electricity, right?) It is funny, though, because the SA group did use retractable needles and really were sham acupuncture. Consequently, the investigators weren't really comparing EA versus the same acupuncture without the current but rather EA to at true sham.
So basically, the groups were as follows: electroacupuncture (EA); standard acupuncture (SA), gabapentin (GP), and placebo pill (PP). There were 120 patients with stage I to III breast cancer treated for cure at the Abramson Cancer Center of the Hospital of the University of Pennsylvania in Philadelphia and with no evaluable disease (i.e., no detectable disease left after treatment) and at least two hot flashes per day for at least a month. They excluded patients with stage IV disease, active breast cancer treatment, initiation or change in hormonal adjuvant therapy within the past 4 weeks, plans to initiate or change hormonal treatment in the coming 14 weeks, pregnancy or breast feeding, bleeding disorders or use of warfarin/heparin, an allergy to or previous use of GP for hot flashes, current use of an anticonvulsant, or documented renal failure in the past 12 months. They were then randomly assigned to one of the four groups according to this schema (click to embiggen):
In any case, the EA and SA groups received their "acupuncture" treatment for 30 minute sessions, twice a week for two weeks, then once a week for six more weeks. Meanwhile, in the GP versus PP groups, the GP group received 900 mg per day of gabapentin or placebo for eight weeks. Outcomes were measured once a week using the average hot flash composite score (HFCS) as measured by the Daily Hot Flash Diary, a commonly used instrument to measure hot flash severity and frequency. Adverse events were also monitored. Patient outcomes were followed for 24 weeks.
Of course, in any acupuncture study, blinding is of critical importance; so whenever you see an acupuncture study, look at the blinding. In this case, monitors blinded to treatment group tallied adverse events (AEs). That's good. The patients were blinded to treatment group between EA and SA and between GP and PP, but were not blinded to whether they fell into one of the acupuncture groups or the medication groups. So was the principal investigators, study investigators, study staff, and the statistician. The acupuncturists, however, were not blinded to whether the patients received EA or SA, which is another huge flaw, almost as bad as the lack of a no treatment control group. In fact, it's bad that they didn't even blind patients between the acupuncture and pill groups. All that would have required would have been to give all the patients in the two acupuncture groups a placebo pill and all the patients receiving pills sham acupuncture and then blind the acupuncturists to experimental group by using a needle that retracts in such a way that the acupuncturist can't tell if it really went into the skin or not (such needles do exist) and then having every patient hooked up to the current generator, which could be set to light up and have its gauge show that it's producing current whether it actually is or not. That way, everyone can be blinded. Then add a wait list/no treatment control. But that's not what they did. I realize my way would be more difficult and expensive, but it is the only way likely to generate anything resembling useful data.
Here's another aspect:
Because placebo response to a pill has been previously reported to be approximately 20%,20 assuming baseline HFCS had a mean of 16 with a standard deviation of 4, we needed 26 participants in each placebo group to detect a 20% difference (3.2 HFCS/day) with 80% power using a two-sided significance level of .05. Assuming a 15% dropout rate, we needed to recruit 30 subjects per arm, for a total of 120 subjects. Our trial was not designed to evaluate the efficacy of EA or GP because sample size requirements would be much larger on the basis of previous literature. Evaluations of the short- and long-term effects between EA and other groups were secondary aims.
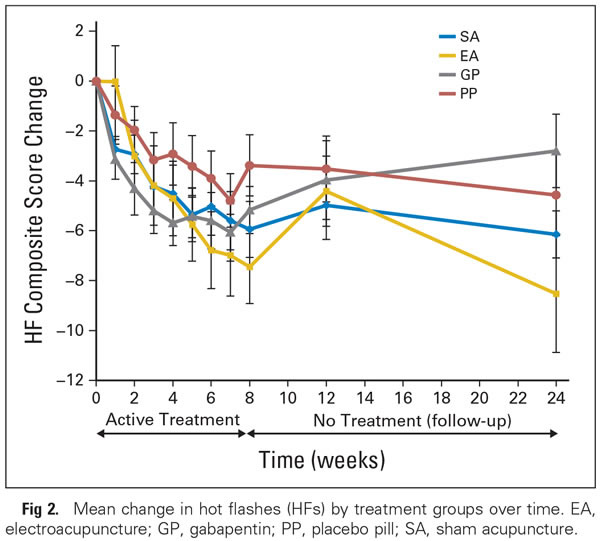
In other words, this study shows nothing about whether EA is actually efficacious, because it wasn't designed to. It's too small. So right away, any results must be interpreted in light of this knowledge, which is why all the discussion of placebo effects. First, however, here is the singularly unimpressive result of the study in the form of a single graph:
First, notice that all groups appeared to be improving right up until the end of the eight week treatment phase and are bunched up. How the authors interpret this result is rather interesting:
By week 8 (end of the intervention), acupuncture produced a significantly greater placebo effect than did pills, with the SA group having a significantly lower HFCS than the PP group (−2.39; 95% CI, −4.60 to −0.17; P = .035). Compared with PP, EA also had improvement in hot flashes (−4.1; 95% CI, −7.0 to −1.3; P = .005), whereas GP showed nonsignificant improvement (−1.8; 95% CI, −3.9 to 0.2; P = .085). We observed differences among treatment groups in the HFCS score (P .001 for time and treatment interaction), with −7.4 for EA, −5.9 for SA, −5.2 for GP, and −3.4 for PP (Table 2 and Fig 2). Participants in the active treatment groups (EA and GP) experienced 47.8% and 39.4% improvement in hot flashes, respectively, compared with baseline. Placebo participants in the SA and PP groups experienced 45.0% and 22.3% improvement, respectively.
So, in other words, everyone improved (which is usually what happens on clinical trials of symptoms with a large subjective component), and somehow the authors see this as evidence that "sham acupuncture" produces a stronger placebo effect than the placebo pills. They also state that the SA group had less nocebo effect (equated with AEs, which I don't consider appropriate given that some of the AEs included bruising In actuality, this might be true, but we really don't know if that's true. For one thing, there is no control group receiving no treatment. How do we know that a no treatment group wouldn't also show a roughly 20% decline in HFCS composite scores just due to the subjects being on a clinical trial? We don't. In fairness, the authors acknowledge this limitation. They also acknowledge that their study wasn't powered to detect efficacy, which puzzled me to no end. Why bother to do the study if it can't demonstrate efficacy? And why say things like this at the end:
In conclusion, acupuncture is associated with enhanced placebo effects and lower nocebo effects when compared with taking pills for hot flashes among survivors of breast cancer. Eight weeks of EA produced promising short- and long-term treatment outcomes for hot flashes compared with other comparators and had fewer adverse effects than GP. These preliminary findings need to be confirmed in larger studies with long-term follow-up. For survivors of breast cancer experiencing hot flashes, acupuncture could be preferable to GP because of sustained benefit after treatment and fewer adverse effects, whereas patients who dislike needles or do not have the time required for acupuncture treatments may prefer GP.
The results with the sham acupuncture, which bested gabapentin, suggest that "there is more than a placebo effect with the sham acupuncture," said Dr. Gary Deng, interim chief of the integrative medicine service at Memorial Sloan Kettering Cancer Center in New York City. "There is a component of behavior of doing a sham procedure, so it psychologically may trigger a different kind of reaction from patients versus taking the placebo pill."
Deng pointed out that clinicians have come to realize that the placebo effect is very important in treatment. "In fact, in clinical practice, every doctor uses it all of the time," he said. "The so-called bedside manner or communication with patients -- all of these enhance the effect of the patients feeling they're getting something."
No one is quite sure why placebos work for some people and not for others, said Deng. "It's like psychotherapy," he added. "Why does it work for some people and not others?" He suggested that differences in anatomy and genetics might be possible explanations, but said "there is a fertile field for further research."
Because the most rigorous studies of acupuncture (and other "complementary and alternative medicine" or "integrative medicine" therapies) are almost always negative and the totality of the literature on acupuncture is consistent with its being a "theatrical placebo," acupuncture advocates, like CAM advocates in general, are now selling it as the "power of placebo." Of course, we know that more invasive interventions produce a stronger placebo effect. For instance, injections tend to produce stronger placebo effects than pills and surgical interventions produce the strongest placebo effects of all. So it would not be surprising if as theatrical a procedure as acupuncture produced a stronger placebo effect than a pill. If you accept that what was measured were placebo effects (and I do not without a no treatment control), then all this study basically showed was that SA is a better placebo than a pill, a result we could already have surmised from the literature, meaning that there was really no need to do this study.
In any event, I've never argued that placebo effects can't be important. However, there is an inherent problem with using them, and that's that you have to lie to the patient, attempts to demonstrate the existence of "placebo effects without deception" that show nothing of the sort notwithstanding. Worse, when a fantasy treatment based on a prescientific understanding of human physiology and disease retconned by Chairman Mao into a seemingly effective therapy is used as the placebo, the message is not so much that we could get the same effects using ethical means of increasing placebo effects, such as good bedside manner, encouraging words, and the like. It's that magic works through placebo effects, which is exactly how this study will be sold.
In the end there are two bait and switches in this study: electroacupuncture sold as acupuncture and acupuncture sold as a powerful placebo that has clinical utility. Same as it ever was.


To my mind, major journals are complicit in this infiltration of quackery into medicine. To cite a recent set of examples, I am beginning to think that there is an effort at PLOS One to pass off acupuncture studies with minimal and inadequate reviews. Otherwise, I cannot find a reason why these studies, with so many glaring lacunae in methodology and interpretations, would find their way into a journal, such as PLOS One:
1. http://www.scilogs.com/in_scientio_veritas/authors-of-plos-one-study-on…
2. http://www.scilogs.com/in_scientio_veritas/cam-peer-review-plos-problem/
3. http://www.scilogs.com/in_scientio_veritas/plos-one-acupuncture-lacks-c…
I did complain rather loudly on Twitter, but I am yet to hear from the PLOS One folks.
Of additional potential concern is the underdosing of gabapentin in this study.
In someone with normal kidney function, the target dose for gabapentin for this indication should be at least 900 mg three times daily. This study used one-third of that dose. If the patient were not having dose-limiting side effects or modified dosing requirements due to decreased kidney function, then that dosing scheme is inadequate.
This is a bit of a side point. But it is a problem that also occurs in pharmaceutical trials as well. (Comparison of one drug to an inadequate dosing of the standard treatment.)
My own practice is to prefer venlafaxine rather than gabapentin as the first choice pharmacologic treatment, all else being equal, due to some (limited) evidence that patient tolerability is higher. http://jco.ascopubs.org/content/28/35/5147.full
I am ashamed that such a great place, where I did two years of fellowship, is promoting such nonsense. At least they had the sense not to offer it to me when I was a patient there. They would have gotten an earful.
In the end there are two bait and switches in this study: electroacupuncture sold as acupuncture and acupuncture sold as a powerful placebo that has clinical utility. Same as it ever was.
Amen.
...are now selling it as the “power of placebo.”
When the health industry starts selling placebo treatments to me is when I start paying them in placebo money.
Yeah, I hope that 1 million dollar check I am going to write them makes them feel wonderful before it ceases to do anything for their bank account.
@Kausik Datta
haha. funny i was just going to link your comment on SBM.
Oh, is that live now? *toddles off to check*
But seriously, for me, both Orac's and Dr. Novella's analyses have separate values. I love Orac's attention to the scientific details.
@ Kausik Datta
"Otherwise, I cannot find a reason why these studies, with so many glaring lacunae in methodology and interpretations, would find their way into a journal, such as PLOS One"
These papers are reviewed by acupuncture experts. Peer review does not make science.
But "hot" papers make high impact.
@Daniel,
"These papers are reviewed by acupuncture experts. Peer review does not make science."
True. To me, that points to a failure of the peer review system, because these reviewers seem to be reviewing acupuncture, and not the science.
This hearkens to what Dr. Novella wrote in the SBM piece: [I quote] "It seems almost that these types of studies are designed not to ask if acupuncture works, but to show that it works..." [End quote]
I suppose the bottom line here is that gabapentin is a pretty crappy drug for treating hot flashes.
Does the paper show the absolute values of HFCS (average, median or range) for each subgroup at time 0? Since a subjective measure like this cannot be linear, especially near the top and bottom boundaries, the subsequent deltas may not be comparable between subgroups.
As a perimenopausal woman, I can vouch that hot flashes can be miserable. Mine have dropped off with time, (and HRT treatment), but for a while I was having 1 ever 1-2 hours. I can't imagine knowing I couldn't treat them - I went flying to the doctor for HRT after the first week of that frequency. I would have tried gabapentin if I'd known that was an option, as I had used it for restless leg syndrome, to see if it worked. But not acupuncture.
These papers are reviewed by acupuncture experts.
This failure mode of peer review is not limited to acupuncture studies, or even medicine in general. It's a particular problem in medicine because medicine is such a large field that it's particularly easy to game the review system.
Here's how it works. The authors will suggest potential reviewers, and the editor will (or should) draw other potential reviewers from (a) his knowledge of who's who in the field and (b) whose papers are cited in the manuscript. The bigger the field, the greater reliance the editor has to put in the latter option. It's too easy for an editor to fail to notice that the literature review in the manuscript is unbalanced (or worse, not care because he agrees with the authors' views), and select reviewers who are sympathetic to that view. Of course the authors' suggested reviewers are likely to be sympathetic as well, which is why only the most foolish or desperate editors will pick more than one reviewer from the list the authors provide.
Also, reviewers can't be expert in everything. So maybe you get a reviewer who is expert on one specific aspect of the paper, and makes the authors improve that part, but overlook some other mistake that would be obvious to an expert in that aspect, but not to the reviewer. This happens routinely in my field, which is a good deal smaller than biomedical fields. I've read several papers in my field which left me thinking, "How the #$&% did that get past the referees?"
Maybe I've forgotten too much of what I was taught about statistics over the last 30 years, but the graph labelled Fig.2 raises hackles. The error bars overlap in all measurements up to 12 weeks, but can then be read as fantastically singular at 24 weeks. What am I missing?
@ Eric Lund
The problem is not related to the field. If one defines "excellence" in science by the number of peer reviewed papers with high short term impact (and two years is very short in science), one should not be surprised to see all this bullshit.
Before giving positions in scientific institutions, it would be better to evaluate individuals on their basic knowledge in the domain and, if possible, their creativity.
And Lo! I have invented a new treatment: Kitten-puncture.
We know from studies like this one that acupuncture is a theatrical placebo, where someone listens to you, and cares about you, and then pokes you a little bit, and you feel better.
Come to my (imaginary) clinic where you'll get a nice cold glass of tea, a big fluffy robe, and then you lie down on a nice soft table with soothing music, and I plop a pile of kittens on your back. It's a pleasant environment, you get stabbed slightly (kitten paws and claws are cleaned between patients) and then you go home.
Now I just need a cat-allergy alternative.
I'd pay money to see how that's done.
Kittens are self-cleansing.
MO'B: Oh, that's easy! First you have them walk across a sticky pad, then dip their little feet in hand sanitizer. The trick is to keep them from licking the sanitizer.
JustaTech - I admit to fairly limited kitting (kitten sounds ungrammatical - see "Elderly Man River") experience. However, the kittings I've known would not willingly walk across a sticky pad nor dip their paws into the entirely inappropriate hand sanitizer (shouldn't it be paw sanitizer? And if so, would that be for male cats only?).
The advocates of CAM love to have it both ways: when criticized that their treatments are no better than placebo, they elevate the placebo to a sort of venerated status, as if it is equivalent to actual effective medical treatments. As has been said often, there is a placebo effect, but the placebo itself has no affect.
If one defines “excellence” in science by the number of peer reviewed papers with high short term impact
I'm aware that it is standard practice to rate journals that way, and I agree it is foolish to do so. I haven't heard of individuals being rated in this fashion, but that would be even more foolish. There is no reason why a good paper shouldn't continue to get citations 10, 20, or even 50 years after publication. There is, however, a reason not to evaluate potential hires on this basis: early-career scientists will not have been in the field long enough to have any ten-year-old papers to cite. And those are the people who are generally considered for assistant professor positions in the US, or the equivalent in other countries.
The pressure for journals to boost their "impact factor" produces a fair amount of pathology. This article is a mild example. It may not mean what the authors think it means, but at least we have no reason to suspect that the described studies didn't happen more or less as described in the paper. Wakefield et al (1998, Lancet) was fraudulent, and there have been many other prominent cases. Nature and Science, which are derisively called "glamour mags" for a reason, are particularly susceptible because they specialize in "hot research" regardless of field; about two thirds of the papers retracted in the wake of the Jan-Hendrik Schön scandal were published in those two journals.
I wouldn't be so sure that kittehs would always avoid sticky surfaces as one of my own willingly ambled across newly varnished- still wet- wood which necessitated a concerted effort on my part in removing said varnish before she licked it or she stuck to something somewhere.
AND my Very Large Cat is quite adept at inserting his own puncturing implements into skin although he knows nothing about meridians.
I'm 50-ish years old, and take gabapentin for neuropathic pain (an approved use) - and I still get hot flashes. Interestingly, I didn't know the drug is used this way, though off-label. I suspect that since the drug makes a person feel drowsy, that the women who are awoken at night time due to hot flashes, find it easier to sleep through them.
This still doesn't explain why the placebo pills have such a marked effect on patients reporting fewer hot flashes (or less severe ones).
@ Eric Lund
The whole process of evaluating science by productivity is insane. And this is why I like quackademics: it's a very good illustration of this.
To Eric "I’m aware that it is standard practice to rate journals that way, and I agree it is foolish to do so."
A two year impact factor was important for librarians in order to know which journals they had to buy. It makes sense. The H index is frequently used by "scientists" to evaluate others. This is stupid and dangerous.
I have a question aboput the following statement:
"the EA is considered the “real” acupuncture and the standard acupuncture (SA) is described as the “sham,”
I don't have access to the paper, but I had a quick look at the protocol (which was available online), and they mention Streitberger needles. To my extent of knowledge, these are supposed to be fake needles that never pierce the skin, but only create the illusion of doing so by hiding in a sheath. Can anyone with access to the paper clarify what type of needles were actually used?
Thanks!
It doesn't matter how robust the evidence is patients are just people that are affraid of pain, loss, death or debilitating illness they are not rational by any means but they are our core buisness. banging this drum is pointless.
Orac,
Would a concisely couched letter to the editor of JCO not achieve your purpose?
ORAC~
A well placed review of a flawed study.
Ii's unnecessary to refer to Jun J. Mao as "Chairman Mao" if even he is the chariman of a dept. or the supporting institution. Reserve sarcasm for you own acquaintances.
I didn't refer to him as "Chairman Mao." I was referring to the real Chairman Mao, who ruled China for decades. Follow the link on his name. It explains all. In fact, it never even occurred to me that Dr. Mao shared Chairman Mao's name, although now in retrospect it's pretty funny to me and I wish I had thought of riffing on Dr. Mao's name in this post.
As for sarcasm, even though there was no sarcasm about Dr. Mao in my post (again, I was referring to the real Chairman Mao from history), I will be sarcastic when and where I damned well feel like it on this blog. If you don't realize that, you obviously haven't been reading very long. I have no intention of changing that.
Not A Troll @ 4: Ouch!, That almost cost me a new keyboard;-) Someone ought to try it as a defence against passing bad cheques. 'That wasn't a bad cheque, it was an acupuncture cheque! An homeopathic cheque if you will, a very good cheque with prosperous financial energy and a most righteous and honourable history!!'
JustATech@ 15: 'Kitten-puncture:' also has the relaxing benefits of a good massage. To get the little moggies to walk across the sticky pad, just place windup mice on the other side of it. A sanitiser gel made from ethanol wouldn't be quite so acutely toxic as one made from methanol, so you'd have time to intervene if they started licking their paws. Just don't make any claims about 'the healing energy of soft fluffy kitties' and we'll recommend you to our friends.
Seriously though, why didn't the nefarious study in question use a TENS arm as a control against EA? Someone needs to do this one: EA, TENS, and a no treatment arm. Thereby demonstrating that any claimed effect of EA is indistinguishable from that of TENS, and removing the magic from the medicine.
@ Lurker
If you remove the magic, then you lose the impact. This paper has been published because of the magic. This blog is popular because of the magic. Orac has published in a high impact factor journal about magic, could he do this with serious issues?
Riard Fitzgerald:
As distinct, I suppose, from you and your friends and acquaintances, who are not at all afraid of pain, loss, death, or debilitating illness? Brave, brave sir Riard.
Most people are afraid of at least some of these things. Some people who aren't actually afraid of pain know that it interferes with most other things, including clear thinking and ability to get things done, even relatively simple things like laundry. I have a relative who tried acupuncture for pain, in the hope that it would let her focus better and/or reduce her doses of narcotics, acetominophen, and NSAIDs. (The acupuncture significantly increased her pain levels, as well as being a waste of money and her limited time and energy.)
Come to my (imaginary) clinic where you’ll get a nice cold glass of tea, a big fluffy robe, and then you lie down on a nice soft table with soothing music, and I plop a pile of kittens on your back
This would be as effective as acupuncture is. Heck, it would probably work better than acupuncture for a lot of people.
I briefly looked around for just such a thing, and didn't find much.
I rather suspect that the EA fanbois don't want to know what we suspect it will show (that is, no difference between EA and TENS), and everyone else suspects it would be a waste of time and money, with little chance of publication.
In 2015, you will find that Acupuncture is both an art and science.
You all are playing around with incomplete concepts and remedies. PLUS you are behind the science. Unfortunately most are behind the science even the schools of Acupuncture.
The art is --- well profoundly well balanced within that time in history, the culture and the real-life observations.
The science is in the book of C. Chan Gunn, MD and an old study done by Cannon Law of denervation.
Gunn lays out the perfect 1 to 1 cause and effect reality based problem + solution = resolution. Muscle pain + the needle as the remedy = resolution of the pain.
If you want more evidence you can study Gunn works. Then you can blend his work into that of Travell, Simons, Rachlin, Hackett et al for the complete 360 view of what is not very observable in the bits and pieces of RCT research.