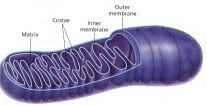
 Last week's Nature had an article on yet another example of poor design: mitochondrial diseases. Mitochondria are the organelles within eukaryotic cells that provide the energy for the cells. Once free-living bacteria, the precursors of mitochondria were engulfed by larger cells billions of years ago. Since that time, mitochondria have lost much of their genome--only 37 genes remain in human mitochondria. Many have ended up in the host nucleus, leaving the mitochondria dependent on the host cell for much of their processes.
Last week's Nature had an article on yet another example of poor design: mitochondrial diseases. Mitochondria are the organelles within eukaryotic cells that provide the energy for the cells. Once free-living bacteria, the precursors of mitochondria were engulfed by larger cells billions of years ago. Since that time, mitochondria have lost much of their genome--only 37 genes remain in human mitochondria. Many have ended up in the host nucleus, leaving the mitochondria dependent on the host cell for much of their processes.
Mutation rates of mitochondrial genes are 10-20 times higher than that of nuclear genes. A main reason for this is that, unlike nuclear genes which are protected in the nucleus, mitochondrial genes are vulnerable to attack from free radicals. At least 30 of the 37 mitochondrial genes have been implicated in disease, several of them progressive and fatal, but generally fairly rare.
However, recent research suggests that mitochondria may play a role in other, more common, diseases as well. Parkinson's disease, progressive-blindness diseases and certain cancers have both been found to involve mutations in mitochondrial genes. More recently, mitochondrial genes have been implicated in type 2 diabetes in individuals who have none of the typical diabetes risk factors.
Typically when a researcher looks for genes associated with disease, we take people who have the disease and people who don't and look at the differences between the two. Some researchers, however, have taken a different approach: determine the proteins necessary for mitochondrial function first, and then look for abnormalities in these proteins in patients. The protein abnormality can then be mapped back to the gene. This methodology has resulted in the identification of hundreds of new mammalian mitochondrial proteins in recent years, and a lot of fertile ground for further research in this area.
Reference: Lane, N. 2006. Powerhouse of disease. Nature. 440:600-2.
Image from http://www.sirinet.net/~jgjohnso/mitochondria.jpg

If there are a lot more mutations in mitochondria, then could mitochondrial mutations be bigger drivers of evolution than mutations in nucleii? And if so, what are the implications of this?
If I've made a non-sensical leap here then please tell me -I'm not a scientist, I just like to read natural history and biology in my free time.
Thanks!
I read that most mitochondria genes are stored in the nucleus along with the nuclear genes and that only about 13 genes are still contained in the mitochondrias themselves. Is that accurate? If that's the case, wouldn't the mitochondria genes be better protected in the nucleus than the 13 genes which are still exposed to the harsh energy production environment?
Sandra, though the mitochondrial genes are more susceptible to mutation, they encode for a much narrower range of protein functions than our nuclear genes--plus, there are only a handful that remain in the mitochondria (37, Alexander, not 12--but close). So it's unlikely that they'd contribute substantially to our overall evolution.
For the last year I have been telling everyone I know that mitochondria and glia are the place to be in medical science. From the tiny bit I know, I am convinced that these two "bits" will provide us with an incomparable understanding of diseases that we think we know a lot about. Thank you for this article as it kind of made me happy to know I was not just talking out of my uneducated but opinionated butt!!
Impatientpatient
I am curious as to why you feel glia are so important? I am quite familiar with MS and it being caused by demylination of the axons in the CNS but am curious as to what other areas you find them significant. Is it specifically the microglia as they are immune cells or the other kinds that mylenate axons such as schwann cells or oligodendrocytes?
My sister (46 years old) has been diagnosed with a Mitochondia disease. Her doctor has said she doesn't know which one. We want to take her to a specialist because her symptoms have been progressing since July 2005 and now are worse. Her symptoms are:
1. Almost complete blindness. Has gotten worse the last 3 weeks.
2. Numbness in finger tips and feet.
3. Chronic low back pain.
4. Her C Spine is inflammed with unexplained fluid at base of brain. The doctor's don't know where the fluid came from. Her spinal tap is clear. No MS. But the doctor's don't know where the fluid came from or what to do about it. They planned a biopsy but cancelled it because they didn't want to operate on her spine.
5. At first they said she had a spine stroke, but now they don't know.
6. She can't walk, can't see, and can't feel. Her trunk area always feels tight.
Any suggestions?
Thank you.
Sylvia
Laura,
Glia are important pain transmitters. The microglia and astrocytes basically set off chain reactions in the immune system, with TNF and other cytokines. Glia are affected negatively by morphine- it irritates them. So in order to control pain more morphine is needed. It is a vicious circle. This is very simplistic, and a researcher Linda R Watkins out of th eUniversity of colorado is the person that I was reading. A good book is Commotion In the Blood- and another good book is Faith Madness and Spontaneous Human Combustion. Both immune system based. Pain- chronic pain- may be in some instances an immune system dysfunction.
That is just off the top of my head, but it has been a very interesting journey over the last few years of researching pain. The view of pain as a choice is a bit Freudian for me and I do not understand why it is still relevant when we can measure cytokines and see the brain with an MRI and stimulate it with electrodes like they do with depression and the wee tiny implant.