I've said this many times before, but it's worth repeating again: whether it's an influenza pandemic, or 'just' annual influenza (which, in the U.S., kills double the number of people as HIV/AIDS), what actually does the killing is the secondary bacterial infection, not the virus.
A recent review describes the result of a large series of autoposies of victims from the 1918 pandemic (as well as later pandemics). The main finding (italics mine):
Their findings are striking in the context of modern conceptions of the 1918 pandemic; the great majority of deaths could be attributed to secondary bacterial pneumonia caused by common respiratory pathogens, particularly pneumococci, group A streptococci, and staphylococci, and not to the virus itself. In fact, although evidence of severe viral bronchiolitis was found, often the primary viral insult appeared to be resolving at the time of the secondary infection responsible for the fatality. Their conclusions are strengthened by the remarkable consistency in theme, if not details, displayed across the many studies reviewed and the inclusion in their review of not only gross pathologic findings but blood and lung tissue culture data. In only 4% of the more than 8000 cases reviewed was no bacterial superinfection documented.
Just to remind people, pneumococci, group A streptococci, and staphylococci are opportunistic commensal bacteria--they often live on and in people, and typically don't cause disease unless the opportunity presents itself. Such as:
necrosis and desquamation of the respiratory epithelium of the tracheobronchial and bronchiolar tree, dilation of alveolar ducts, hyaline membranes, and evidence of bronchial and/or bronchiolar epithelial repair.
And lookee, a figure:
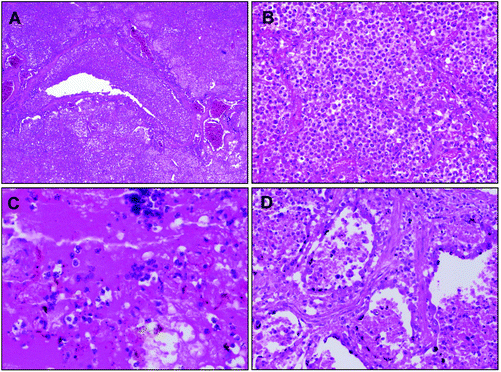
Figure 1. Examples of hematoxylin and eosin-stained postmortem lung sections from 4 victims of the 1918-1919 influenza pandemic (see text). A, Typical picture of severe, widespread bacterial bronchopneumonia with transmural infiltration of neutrophils in a bronchiole and with neutrophils filling the airspaces of surrounding alveoli (original magnification, 40Ã). B, Massive infiltration of neutrophils in the airspaces of alveoli associated with bacterial bronchopneumonia as in A (original magnification, 200Ã). C, Bronchopneumonia with intra-alveolar edema and hemorrhage. Numerous bacteria are visible both in the edema fluid and in the cytoplasm of macrophages (original magnification, 400Ã). D, Bronchopneumonia with evidence of pulmonary repair. The alveolar epithelium is hyperplastic; interstitial fibrosis is seen between alveoli (original magnification, 200Ã).
(I don't really understand all of this; I'm Mike the Mad Biologist, not Mike the Mad Histopathologist. It is very purple, however, and you don't want your lungs to be purple, do you?*)
Back to the review. The author notes (italics mine):
This homogeneity in findings reinforces the idea that the end result, death from bacterial pneumonia, is a common feature of all pandemics in the preantibiotic era. If this supposition is correct, the virulence of the virus itself may not be the key predictor of mortality; the ability to interact with bacteria may be the more important factor. In this light, the study of virulence factors that increase the incidence or enhance the case fatality rate of secondary bacterial infections is as important as understanding the basic biology of influenza viruses with pandemic potential.
Given the importance of bacterial infection, you can bet that a lot of antibiotics are going to needed and used (italics mine):
Even if a clinical course similar to our recent H5N1 experience occurs in the next pandemic, our ability to provide modern intensive care and administer broad-spectrum antibiotics will certainly be compromised if clinical attack rates approach the 25%-30% range seen in previous pandemics. In this scenario, bacterial infections are likely to emerge as a major complication in survivors of the primary influenzal disease....
Planning for prevention of disease must include pneumococcal vaccines as well as influenza vaccines. A comprehensive survey of the sources, supply, and surge capacity of important antibiotics should be undertaken. This should include analysis of distribution patterns, as has been done for influenza vaccines; it is likely that many of the countries in the developing world, where complications of pandemic influenza are likely to be worst, will have little to no access to appropriate antimicrobials in this scenario. Planners should consider strengthening and diversifying these pipelines--in the United States alone in the last 3 years, there have been shortages of more than a dozen antibiotics. Included among these is vancomycin, an important drug used in the treatment of antibiotic-resistant infections due to Streptococcus pneumoniae and Staphylococcus aureus, the 2 most common secondary pathogens in the infections that follow influenza.
As I've mentioned before, bacterial vaccines are critical in limiting influenza-related deaths, and we don't use them the way we should.
What's frustrating about our lack of a coherent influenza policy--which is even more obvious in our inability to combat the annual influenza epidemic--is that we know what to do and how to do it: vaccination and stockpiling antibiotics. Yet, as a nation, we are politically incapable of doing so. All of that anti-vax garbage doesn't help either. More maddening is the fact that all of these steps could be used for both a pandemic and the annual epidemic.
Yet we do nothing. No doubt, in May or so, I will have the joy of writing another outraged post about the 36,000 dead people (give or take), most of whom would not have died if we actually had an anti-influenza policy.
*I'm kidding. The purple is from the chemical stain used.

Not to mention the US stealth policy of denying flu vaccine to countries on its evil enemies list (North Korea is on it despite being officially removed from the terror list). Link at my name to action follow-up links post.
'Planning for prevention of disease must include pneumococcal vaccines as well as influenza vaccines. A comprehensive survey of the sources, supply, and surge capacity of important antibiotics should be undertaken.'
FYI... Our group here is doing just this.
Brilliant idea, review studies done at the time and see what the doctors with the first hand access to recently dead patiens diagnosed. It only makes sense.
But it has one enormous flaw. Those doctors had no knowledge of the influenza virus--it wasn't even discovered yet. The entire concept if viral biology was only 2 decades old. And just because bacteria were present and could be cultured doesn't necessarily mean that they were the cause of death.
The fatal flaw though is not understanding the significance of why influenza infections such as H5N1 and the 1918 flu killed predominantly healthy adults instead of the usual pattern of children and the elderly. It is precisely because the cause of death was not a bacteria taking advantage of the weakened immune system of a flu victim whose immunity was already compromised. Rather this indicated the over-reaction of a healthy immune system causing resperatory failure, with stronger immune systems able to over-react more catastrophivally--the so-called "cytokine storm."
thanks
thanks