
I'm kidding, but ScienceBlogling Tara Smith has co-authored a PLoS One article about the emergence of the MRSA strain ST398 in Iowan pork farms. Pig farms are a tremendous reservoir of bacteria: as far as I can tell, there are about six pigs for every person in Iowa.
MRSA ST398 a methicillin resistant S. aureus bacterium that has spread epidemic through various European animal populations (particularly pigs). It recently jumped from the animal population to the human population in Europe and has begun to establish itself there in hospitals. The last thing we want is for another MRSA strain which is good at colonizing clinical setting to increase in the U.S.: we have enough problems with MRSA USA200 and USA300, thank you very much....
Which leads us to Tara's article. I'll get to my thoughts and questions in a moment, but I'll let the article's abstract summarize the findings first (unlike too many articles, the abstract actually does its job; I've added a couple of notes to explain some technical things):
Background
Recent research has demonstrated that many swine and swine farmers in the Netherlands and Canada are colonized with MRSA. However, no studies to date have investigated carriage of MRSA among swine and swine farmers in the United States (U.S.).Methods
We sampled the nares of 299 swine and 20 workers from two different production systems in Iowa and Illinois, comprising approximately 87,000 live animals. MRSA isolates were typed by pulsed field gel electrophoresis (PFGE) using SmaI and EagI restriction enzymes, and by multi locus sequence typing (MLST). PCR was used to determine SCCmec type [Mad Biologist: methicillin resistant gene type] and presence of the pvl gene [Mad Biologist: pvl stands for Panton-Valetine leukocidin, which kills blood cells; it may or may not result in increased disease severity].Results
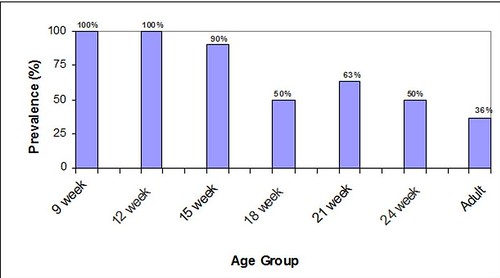
In this pilot study, overall MRSA prevalence in swine was 49% (147/299) and 45% (9/20) in workers. The prevalence of MRSA carriage among production system A's swine varied by age, ranging from 36% (11/30) in adult swine to 100% (60/60) of animals aged 9 and 12 weeks. The prevalence among production system A's workers was 64% (9/14). MRSA was not isolated from production system B's swine or workers. Isolates examined were not typeable by PFGE when SmaI was used, but digestion with EagI revealed that the isolates were clonal and were not related to common human types in Iowa (USA100, USA300, and USA400). MLST documented that the isolates were ST398.Conclusions
These results show that colonization of swine by MRSA was very common on one swine production system in the midwestern U.S., suggesting that agricultural animals could become an important reservoir for this bacterium. MRSA strain ST398 was the only strain documented on this farm. Further studies are examining carriage rates on additional farms.
One interesting observation is that younger piglets were more likely to be colonized than older piglets and adults:
It might be that as the immune system of pigs matures, they are more able to fight off MRSA 'infections' (which, in this case, don't cause disease in pigs). Antibiotic resistance in these Iowan ST398 isolates is unusual too: many are resistant to clindamycin, but not erythromycin. This is a very odd phenotype and suggests a novel genetic resistance mechanism.
A final interesting section from the paper:
Additionally, a portion of the sows at PSA were imported from Canada, while those from PSB originated in Michigan. Canada is the most important exporter of live hogs to the U.S. Thus, it is possible that ST398 may have been brought into the U.S. via live swine or pork products. However, this study was not designed to identify the source of the MRSA and additional research should further examine this question.
Blame Canada? Actually, some detailed genomic sequencing could get at this. Too bad that there's no one who's interested in this question who is in a position to attempt to get projects like this funded.
Just saying.
Anyway, the whole paper is worth a read--and I think is very accessible to the non-specialist reader.

Antibiotic resistance in pathogenic bacteria is a widespread and troubling problem. The main mechanism for bacterial resistance is the production of beta-lactamase enzymes which catalyze the hydrolysis of the antibiotic rendering it ineffective. Bacteria are asexual and don't mate; however, they are promiscuous with pieces of DNA called plasmids. Antibiotic resistance in new strains of bacteria is often due to plasmid sharing.
To combat and slow bacterial resistance a radical shift in production farming technique will have to occur... that is farmers will have to stop the widespread use of antibiotics in livestock feeding. Furthermore, when it comes to clinical practice physicians and patients must stop prescribing/demanding antibiotics for everything.
Cynthe,
While some resistance genes in S. aureus are plasmid-encoded, the methicillin resistance genes are chromosomal. But you're right, for many of the beta-lactams and other resistances (chloramphenicol, florfenicol, sulfonamides), plasmids do play a big role.
I'm curious - how much would it cost for farmers to stop using antibiotics without clear medical need? Similarly, how much does MRSA increase health-related costs?
(However - MRSA costs are as far as I know very unpredictable, both in the sense that a individuals who get sick often pay high costs (possibly including death), and in the sense that an epidemic would have extraordinary costs. In contrast the cost of not using antibiotics for non-medical needs probably only results in animals that grow slower - a highly predictable cost increase. So I don't expect a naive cost comparison would help decide whether antibiotics should not be used for non medical needs. At the very least the character (money can't undo death or other kinds of permanent health damage) and predictability of the cost would need to be included. But I'm not a deciderator, I'm just curious.)
As a health researcher who has worked in hospitals with MRSA problems and doesn't ever want to become a surgical patient,I would love it if farmers bred animals who were disease resistant and stopped using the bl**dy antibiotics! Maybe with advances in gene research they'll be able to alter or implant resistant genes for use in artificial insemination programs?? Why can't someone do a PhD on the DNA sequencing between Canadian and Iowa pigs?? No eager students and someone with a grant there?
It's not cheap--we have a 454 system at the University but for microbial genomes it's still 10k/pop.
llewelly,
There's an additional reason for using antibiotics, which is to prevent disease outbreaks (in poultry, for example, flocks can be wiped out almost overnight). Denmark, for instance, bans antibiotic use, but compensates farmers for lost flocks. I don't know to what extent this is an issue in swine.
What makes it harder is to determine what role agriculture is playing; the ag lobby has successfully prevented surveillance programs from comprehensively looking at this. Nonetheless, MRSA infections are very costly. In MA, the average treatment cost of an MRSA infection is >$48,000 (sensitive infections are $7,000). Since MRSA is a breakdown of infection control, basically the cost is, well $48K. However, we don't know how much of this is due to agriculture.
Kay,
Actually, to sequence a pig genome would be much more expensive than Tara suggests (and would take at least a year). Once the genome is sequenced, hunting for genetic variation (which is fraught with difficulties) would be expensive to do across thousands (many thousands actually) of pigs.
Thank you, Mike, but what do you mean by '(sensitive infections are $7,000)' ?
llewelly,
sensitive infections cost, on average, $7,000 to treat in hospitals (remember, that's the average; many will be less, some will be much more).
I would think that another way to decrease the need for antibiotics in farm animals would be to improve their immune system. The easiest way to do that is to increase the amount of time animals are kept with their lactating mothers. Everything I have read about human milk sugggests that one of its main purposes is to act as a primer for the immune system. For example the thymus gland (which encourages the production of mature T cells)is twice as large in breastfed babies as in those fed artificial formula- Lars Hanson "The Immunobiology of Human Milk").
Domestic animals (including humans) are routinely weaned much earlier than nature intended which deprives them of the chance to develop a thriving immune system. They can survive yes, but their immune system is not as well devloped as it would be otherwise.
As I said one of the problems is domestic animals are weaned too early. When my cat had a litter the vet insisted that the kittens should be weaned at 6 weeks. I kept the mother & kittens together and they continued to nurse for a full 6 months! If we keep mothers & offspring together longer we may be able to decrease the need for antibiotics especially in young animals.
I know this isn't a high tech answer, but sometimes getting back to basics lets you see a problem in a new way. Any comments?
Kathy Abbott, IBCLC
Regarding the first comment on plasmids, etc., given how often phage jump in, out and around S. aureus genomes, chromosomal resistance elements can certainly be transfered between strains. Granted, a whole SCC mec element isn't going to move at once, but I'm not sure you need all of it to get some form of methicillin resistance. For example, great work by the Tomaz group just described how pbp4 jumped from S. sciuri to S. aureus (http://aac.asm.org/cgi/content/abstract/53/2/435)
Anyway, I hope someone sequences ST398 soon. I'm dying to know what it looks like, or more specifically, what other strains look like it (if any).
weaned much earlier than nature intended which deprives them of the chance to develop a thriving immune system. They can survive yes, but their immune system is not as well devloped
very thanks for article
As a health researcher who has worked in hospitals with MRSA problems and doesn't ever want to become a surgical patient,I would love it if farmers bred animals who were disease resistant and stopped using the bl**dy antibiotics! Maybe with advances in gene research they'll be able to alter or implant resistant genes for use in artificial insemination programs?? Why can't someone do a PhD on the DNA sequencing between Canadian and Iowa pigs?? No eager students and someone with a grant there?