 A few weeks back during the whole Egnor kerfuffle, I mentioned how important an understanding of evolutionary biology was to many areas of epidemiology, and specifically, for vaccine development and implementation. As one example, I brought up the phenomenon of serotype replacement, which can occur due to the use of what are called "multi-valent vaccines." Essentially, these vaccines include strains of pathogens which are either the most common, or the most likely to cause disease--thereby protecting individuals from infection with these specific serotypes, but not making the recipient immune to infection with other strains that aren't included in the vaccine formulation. The concern is, then, that once those types are reduced in the population via vaccination, other serotypes can come along and fill the niche that they've vacated. A recent story by Helen Branswell notes that this is exactly what's happening with pneumococci:
A few weeks back during the whole Egnor kerfuffle, I mentioned how important an understanding of evolutionary biology was to many areas of epidemiology, and specifically, for vaccine development and implementation. As one example, I brought up the phenomenon of serotype replacement, which can occur due to the use of what are called "multi-valent vaccines." Essentially, these vaccines include strains of pathogens which are either the most common, or the most likely to cause disease--thereby protecting individuals from infection with these specific serotypes, but not making the recipient immune to infection with other strains that aren't included in the vaccine formulation. The concern is, then, that once those types are reduced in the population via vaccination, other serotypes can come along and fill the niche that they've vacated. A recent story by Helen Branswell notes that this is exactly what's happening with pneumococci:
Two new studies from Alaska and from Spain suggest that serotypes or strains of pneumococcal bacteria not covered in the vaccine -- sold as Prevnar -- are stepping into the void left by those the vaccine protects against."I think we knew there was that potential for that to occur, but there was no way to predict if it would occur or to what extent," Dr. Rosalyn Singleton, lead author of the first study, said from Anchorage.
As Singleton notes, it's difficult to predict exactly what will happen when such a niche suddenly is available. Because strains that cause disease tend to get the bulk of attention (and research dollars), typically less is known about the rarer serotypes of pathogens. Are they rare because they've simply been out-competed for some reason by the more common strains? Are they inherently less virulent, and therefore unable to cause as much disease in humans? It would appear that the latter is not the case, at least for the pneumococcus (Streptococcus pneumoniae):
In Alaska, rates of invasive or serious pneumococcal disease among native children went from 403 per 100,000 children a year before the vaccine to 134 per 100,000 after the vaccine was introduced in 2001.
But that figure rose again to 245 per 100,000 by 2004-2006, with the bulk of cases -- 229 per 100,000 -- due to pneumococcal strains not included in the vaccine, the Singleton article reports.
The Spanish study, by researchers at the University of Navarra, also showed an upswing of cases caused by non-vaccine strains after immunization with Prevnar began.
Note that this doesn't mean the vaccine isn't successful. Rates of invasive disease even in the recent years are still about half of what they were before widespread use of the vaccine, so that's still a lot of morbidity and mortality avoided. And Wyeth, maker of Prevnar, is already working on updating that vaccine as the epidemiology of the strains circulating in the population changes (which is what we already do, in essence, yearly with the influenza vaccine). However, careful surveillance and a good understanding of the ecology and evolution of the bacterial species (as well as its interaction with other species who could potentially fill the same niche) will be critical to maintaining a level of success in these fast-moving pathogen populations.
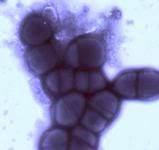
Image from http://www.hpa.org.uk/infections/topics_az/pneumococcal/images/blue2.JPG

Interesting. I've known about the dynamic of disease and prevention for some time, but this is a good, concise example of a specific case. Or cases.
From what I've seen of denialists of modern medicine (on this and other science blogs), this is an example of what they see as a failure of their definition of "science". But if one actually reads the post and pays attention, it is a vindication of the scientific process.
I had noticed the Alaska and Spain studies, too. As you say, pneumococus vaccine has had an impact on invasive disease, but serotype niche-snitching is an important issue for vaccinologists to keep an eye on. Interestingly-- and I don't have citations here--haemophilus influenzae type A strode into the niche held by type B before widespread HiB vaccination of kids started in the late 80s/early 90s. HiA is a less virulent organism, though, so it's "all good."
The thing that wasn't clear to me was whether the CDC/AAP et al were aware of the serotype replacement possibility before they started the HiB program. I haven't gone over teh paper trail but I kind of doubt it. It's all sort of serendipitous. Luckily, we've been lucky.
On a related note, there were debates before the introduction of rubella, and most recently chickenpox vaccines, about whether vaccination of babies and toddlers would push the disease burden into older people, who more likely to get sicker (and have repercussions like congenital rubella syndrome). This didn't happen with rubella -- with chickpox there's been quite a lot of breakout disease so the CDC's ACIP is recommending a second dose.
Arthur Allen, author, "Vaccine, the Controversial Story of Medicine's Greatest Lifesaver." (WW Norton)
Hi Arthur,
Non-typeable Hi as well, which also (as far as we've seen thus far) haven't yet been as nasty as serotype B either. I'm not sure myself about what was done before widespread introduction of the vaccine, but I find it tough to believe they didn't consider it. I'll have to check that out sometime.
I just recently learned that human rotaviruses are believed to be responsible for roughly 20% of infant diarrhea deaths in the world, some half a million infant deaths per year. A few vaccines have already been produced, and tested. I was afraid, when I read the title of your post today, that you would be talking about reassortment of chromosomes between vaccine strains and pathogenic strains in this type of virus (rotoaviruses and influenza viruses have genomes with several genetic segments equivalent to chromosomes).
I am not familiar enough yet with the vaccines and the human rotaviruses, to know if there is any risk of reassortment. I suspect that any such risks are absolutely trivial in comparison to the risks of non-vaccine rotaviruses from humans or other species reassorting "in the wild".
The rotaviruses are a very interesting group, with extreme diversity and some species specificity. It is interesting that simply using developed world sanitation systems to provide clean water etc. does not eliminate them. Rotavirus infection causes much infant diarrhea in the USA and Europe, but kills infants less frequently because of better treatment of cases.
References:
Parashar UD, Hummelman EG, Bresee
JS, Miller MA, Glass RI. Global illness
and deaths caused by rotavirus disease in
children. Emerg Infect Dis 2003;9:565-
72.
Bresee JS, Glass RI, Ivanoff B, Gentsch
JR. Current status and future priorities for
rotavirus vaccine development, evaluation
and implementation in developing countries.
Vaccine 1999;17:2207-22.
Buttery JP, Kirkwood C.
Rotavirus vaccines in developed countries.
Curr Opin Infect Dis. 2007 Jun;20(3):253-258.
PMID: 17471034
Clark HF, Offit PA, Plotkin SA, Heaton PM.
The new pentavalent rotavirus vaccine composed of bovine (strain WC3) -human rotavirus reassortants.
Pediatr Infect Dis J. 2006 Jul;25(7):577-83. Review.
PMID: 16804425
OK, non-biologist here, just your everyday software engineer/electrical engineer. Is there someone that can point me to an article or paper that more carefully explains the idea of an "empty niche" in respect to pathogens? Also, what is the theory behind pathogen competition? What exactly are they competing for? How does a successful pathogen "win" against another?
I'm looking at going into bioinformatics and I'm trying to build up a background knowledge, so any good information that you can give me would be most appreciated.
"Note that this doesn't mean the vaccine isn't successful. Rates of invasive disease even in the recent years are still about half of what they were before widespread use of the vaccine, so that's still a lot of morbidity and mortality avoided."
Yeah, but at what cost? When this vaccine was released, the CDC figured it would be cost effective at (IIRC) about $48 a dose. The company sold it at $56 a dose, so it wasn't cost effective at the outset. Now, as the effectiveness is dropping, it is selling for over $80 a dose. When do we get to say the benefits aren't worth it anymore?
-RR-