I'm conflicted about Nicholas Kristof's recent op-ed about antibiotic resistant organisms. On the one hand, Kristof is one of the only national columnists to raise this issue at all. On the other hand, I found his most recent column somewhat confusing--and I'm an expert in this area (I also think he's jumping to unfounded conclusions, but more about that later in the post). I think this is largely an effect similar to playing "telephone": information is being transferred multiple times from the primary source and finally conveyed by someone with no biological training. So what I'm going to do in this post is lay out some of the basics, as well as touch on a couple of specifics in Kristof's op-ed.
First, let's talk about E. coli (the full species name is Escherichia coli). I know a thing or two about E. coli (among other things, I'm involved in the effort to sequence 100 E. coli genomes). E. coli is a commensal bacterium--that is, it lives in you without causing disease*. It typically lives on the surface of your colon, which is part of the intestinal tract (presumably this is what Kristof means by "in the colon). We all have E. coli, and some happen to be resistant to one or more antibiotics, even if you haven't used antibiotics for a long time (or ever). Usually, there's a dominant strain (genotype), and it can persist in people for weeks or months, then it is replaced by another strain of E. coli. While some people can be colonized for a very long time ('shedders'--Typhoid Mary was permantly colonized by Salmonella, a relative of E. coli). Most birds and mammals are colonized by E. coli too, and reptiles and fish can also have E. coli. (All of this will be important when I get to agriculture. You will be quizzed).
Onto MRSA, which is short for methicillin resistant Staphylococcus aureus. Let's deal with the "SA" first. S. aureus, like E. coli, is a common commensal (look to your left, look to right, one of you three will have S. aureus). It typically lives up your nose, and in other moist places:
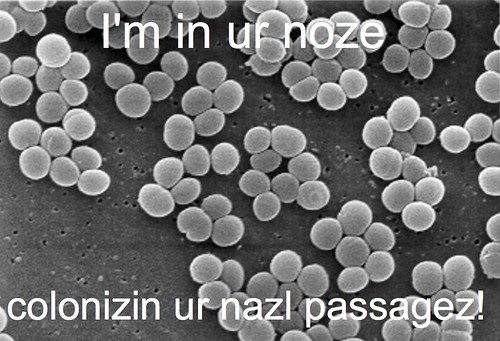
Like E. coli, S. aureus can also colonize mammals and birds (the 'piggy MRSA', ST398, is one such example).
OK, one more bit of Antibiotic Resistance 101. Since we just finished with S. aureus, let's move on to methicillin resistance (the "MR" in MRSA). Methicillin is a derivative of penicillin, and methicillin resistance typically confers resistance to most antibiotics derived from penicillin (these antibiotics are called beta-lactams). MRSA typically is treated with vancomycin, as it's the only antibiotic guaranteed to work (most of the time anyway), although some MRSA are sensitive to other antibiotics**. One more point about beta-lactam antibiotics (penicillin and its derivatives): they are effective against E. coli too. But E. coli and its relatives typically use a different type of resistance known as extended-spectrum beta-lactamases, or ESBLs. ESBLs differ in which beta-lactam antibiotics they confer resistance to--the most dangerous ESBLs, known as KPCs (which I've discussed before), confer resistance to all beta-lactams. And of course, these ESBLs usually co-occur with genes that confer resistance to other classes of antibiotics, making them virtually impossible to treat (the only available therapy involves the use of colistin which can cause organ failure. Also, colistin resistance evolves very rapidly).
Finally, let's deal with disease very briefly. These commensal bacteria usually don't cause disease, but when they wind up in a usually sterile site, such as your bloodstream, they can cause disease (which appears to have happened in the case Kristof discusses in his op-ed). But this is an unusual situation*** (it also helps if you're immunocompromised). In other cases, some bacteria cause disease in humans, but not in other host animals (e.g., E. coli O157:H7 doesn't cause disease in cattle, but it does in people).
I brought all of this backgroup up because Kristof brings up the role of agricultural (mis)use of antibiotics. Long-time readers will know that I think the misuse of antibiotics in agriculture is a serious problem. Hell, professionally, I've worked to ban the use of cefquinome in cattle. I've got bona fides here. Regarding misuse, it's pretty clear that agricultural misuse of avoparcin on farms led to the evolution of vancomycin-resistant enterococci (enterococci are another group of commensal bacteria) which then entered the European hospital system (this antibiotic was never approved for agricultural use in the U.S.--yes, sometimes we don't fuck up regulation...). Another example is the Portugese misuse of nitrofurantoin, which is used to treat urinary tract infections.
But regarding ESBLs in E. coli (and related bacteria) and MRSA, the situation is more complex than Kristof makes it out to be. There's little evidence that ESBLs arose on the farm and, then, entered clinical settings (i.e., hospitals). Nonetheless, use on farms can serve to amplify or maintain ESBL-possessing organisms. That is, the farm can serve as a reservoir of resistant organisms and resistance genes. In fact, we are starting to observe increases in ESBLs in commensal bacteria isolated from the farm; however, that increase trailed the rise in the clinic. MRSA is more complicated. It's pretty clear that methicillin resistance evolved in the clinic, and spread worldwide (multiple times, in fact). But methicillin resistance has since transferred into a S. aureus strain (ST398) and is spreading globally in pigs. In Europe, this strain has now entered hospitals at low frequencies. Here, it arose in the clinic, spread into agricultural strains, which are now 're-entering' the clinic.
So, should we be limiting the use of antibiotics in agriculture? Absolutely. But, with regards to ESBLs and most MRSA, we also need to improve infection control at hospitals. That means strict isolation and screening of patients and staff, since much of the original amplification*** of the ESBL and MRSA problem appears to first happen in hospitals.
*And on you. And on human-associated surfaces. You really don't want to know what's living on your toothbrush....
**One of the issues with a life-threatening antibiotic resistant infection is that you need an effective treatment now, not in 48-72 hours. There may not be time to figure out which antibiotics work; you need the 'magic bullet' immediately.
***There are some lineages of E. coli which seem to be primarly pathogenic (i.e., no non-human commensal hosts have been found).
****I use the phrase amplification, since it's not clear where resistance first evolves. But for the cases of ESBLs and MRSA, they were first observed (and increased rapidly) in hospitals, not farms (as I noted, other forms of resistance arose first on farms and spread to hospitals--it's not either-or).

On a different, yet not unrelated, note, did you ever see this paper, which appeared back when I was working in the HGT field:
A Salmonella enterica serovar Typhimurium strain that harbored a plasmid carrying a TEM-1-type β-lactamase gene was isolated from the blood and cerebrospinal fluid of an infant with meningitis. This 3.2-kb plasmid was further characterized to be a nonconjugative pGEM series cloning vector containing a foreign insert. The strain was likely laboratory derived and contaminated the environment before it caused the infection.
Rather depressing, though fortunately there aren't so many reported incidences such as in the literature.
Agreed. I find Kristof tends to get things just wrong enough on medical issues.
Also, there is a significant difference between hospital-acquired and community-acquired MRSA, with CA-MRSA usually being susceptible to several common oral antibiotics.
Scary as it is, the contribution to microbial resistance is the collective effort of individual doctors guided by the CYA (Cover Your Ass) directive. In a society obsessed with safety as well as litigation it is easy to blame a specific case of illness on a perceived failure to prescribe (the correct) antibiotics, but it's impossible to trace antimicrobial resistance back to all the instances of inappropriate drug use that contributed to it.
Rational use of antibiotics was already a big issue during my veterinary education, and then you go out into the "real world" where each practice has it protocols as well as revenue from drug sales, and pop goes your idealism. So there is something to be said for life in the ivory tower, where people can afford to say that the best treatment for wounds is unpasteurized honey!
I asked this question once before and got no response:
What happens to the hospital staff who harbor S. aureus? or other bad bugs? Do they lose their jobs? Are they forever banned from working in hospitals? Or, can they be cleared of the offending organisms?